
Why spend hours on the phone with payers when you can check online in minutes?

Why spend hours on the phone with payers when you can check online in minutes?

The toughest payers to collect from are your own patients. Don't despair, there are things you can do to get paid.

The future of the direct-pay practice model is bright. Here's how it works, the affect on patients, and where it fits with models promoted by healthcare reform.

Today's practice managers must plan proactively for the new year - finding new ways to cut costs and improve efficiencies.

When patients demur over paying for care, don't be a soft touch - there are things you can do to collect

Medical coding guidance on prevention planning; the ICD-10 transition; ABN advice; and more.

The deadline for conversion from the present electronic claims transaction standard to Version 5010 is fast approaching. Make sure both your practice and systems vendor are ready for the change.

Medical practices face two significant deadlines that require planning and testing in 2011. The first is the new 5010 electronic claims transmission standard, the second ICD-10.
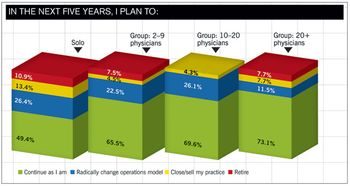
According to our 2010 Physician Compensation Survey, group size can be a big factor in how much you earn. Find out how your income stacks up to that of your peers.

Thinking of selling your practice and getting a job with a hospital? Here's some advice for doing it right from experts who negotiate the deals.

I’ve found the most important factor in deciding between in-house or outsourced billing to be that of your management style.

Here are some simple things you can do to help boost your revenue.

Chances are you are going to get audited in the next few years. But don’t panic - use our audit guide to get your practice prepared instead.

Even if you choose not to implement a full EHR right now, you can take a big step toward digitizing your practice.
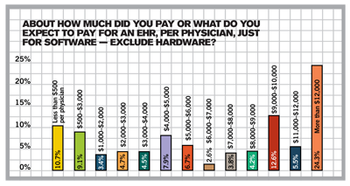
If you’re confused about the federal incentives to buy an EHR and what meaningful use means, you're not alone. We have the answers in our 2010 Technology Survey.

Advance preparation is your key to successfully managing the ICD-10 conversion. Here’s what your practice needs to know and do to get ready.

Here’s how to skip the drama and hire right the next time at your medical practice.

If you can't verify a patient's insurance, their signature on this form shows they know they are responsible for payment.

CMS has released its proposed changes. Not sure how it will impact you? Have a gander at this. It'll give you what you need to prepare. We took it straight from the horse's mouth, straight from the proposed regulations.

Follow our flowchart to find ways to improve your collections. A great companion to our Accounts Receivable Key Indicators calculator. If your results there are lower than you like, this flowchart will help you improve.

Medicare denies claims for 26 percent of all services submitted. More distressing -- 40 percent of those services are never resubmitted for payment by providers. Talk about missed opportunities! Customize this form letter -- and the ones below -- to appeal claims denied, no matter who the payer is. Use this letter to show payers that the claims you are sending are not dups, but corrections.

This is similar to the general notice above, but is specifically for laboratory work. Again, this form comes directly from the Center for Medicare and Medicaid Services. Access its Web site for more information.

Compare your denial rate from Medicare to national averages for your specialty by total amount denied, number of services denied, or percent of services denied. Data from the Centers for Medicare and Medicaid Services.

Manage your denials from insurance companies by tracking them in this worksheet. Track the denials according to the functional area to identify opportunities for improvement. By tracking and monitoring denials, you can fix the problem and prevent denials in the first place.

This simple work sheet will let you compare your payers' reimbursement for specific procedure with your costs for each procedure. If you're spending more to provide a service than you're making for it, then it's time to address the problem.