
The government has some ideas about what’s wrong with Medicaid, and how to fix it. Too bad their ideas don’t have much to do with paying doctors better.

The government has some ideas about what’s wrong with Medicaid, and how to fix it. Too bad their ideas don’t have much to do with paying doctors better.
We hear you. Unfortunately, physician reimbursement continues to decline, according to the results of our exclusive 2007 Fee Schedule Survey. That’s the bad news. Now here’s the good news: Along with all the hard data, we arm you with the tools you need to fight back.

When asked to a see a patient by another physician, does it really matter if you bill an E&M visit as a consult or a referral? It sure does - and using these terms interchangeably can cost your practice thousands. We help sort out the differences.

You deserve every penny you’ve earned. But if your practice is like most, you probably aren’t getting that. There are technologies out there that can help - but which one is right for you?

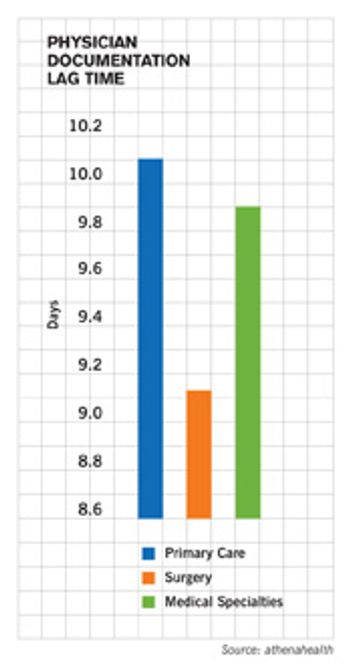
Your days-in-A/R report tells you how long it takes you to get paid - and the longer it takes, the more it costs. Learn how to read these reports correctly so you can fix whatever’s holding up your checks.

A Texas psychiatry practice gets help finding its backbone in dealing with negligent payers.

Patients are increasingly asking doctors to keep diagnoses and treatments out of their records to avoid damaging their chances of obtaining insurance coverage in the future. What should you do?

Tired of being judged by payers? Here’s your chance to turn the tables and judge them. With help from our friends at athenahealth, we give you the second annual PayerView rankings. It’s a report card that uses real claims data to judge dozens of local and national payers on how well they treat you, the physician. Compare this data with your own; then strive to change what isn’t working.

More of your practice’s revenue is coming directly from patients. Better bone up on your collections processes.

We know you don’t like insurance companies. They’re bureaucratic, inefficient, faceless. But to get paid better and faster, you’ll have to learn to work together. And they have a few ideas on how to make that happen.

Another selection from our weekly e-mail newsletter. This issue: how to handle Medicare denials.
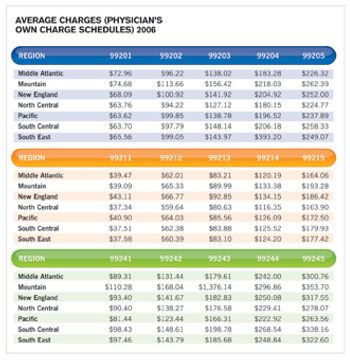
This is the toughest year for physician reimbursement since we started surveying you on your fee schedules in 2001. Still, there are some ways to fight back.
What should you do when your reports indicate a billing problem?

Analyzing your revenue trends.
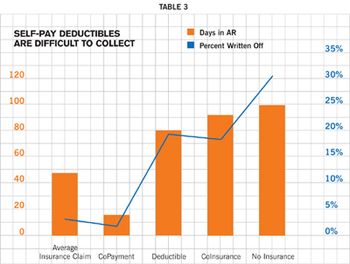
Handling self-pays.

Medicare and many private insurers have been marketing their pay-for-performance programs as “free money” for good doctors. But beware hidden costs.
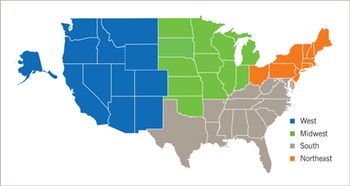
Fed up with payers who deny claims unreasonably, inexplicably lose them, or just take too long to pay? It's high time you did something about it. And now - finally - you have the information you need to act. Welcome to PayerView, the first-ever data-driven payer ranking based on how easy - or difficult - they are to work with.
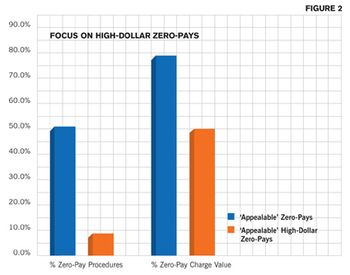
Underpayments and "zero-pays" are a growing problem. Here's some advice to help you handle them.

Evaluating a payer contract requires more than a working knowledge of the fee schedule. If you want to negotiate a better deal when it's renewal time, you need to know how each payer does business.

Worrying about whether your coding and billing practices are within the law can keep you awake at night. We offer some guidelines to help you stay on track.

Here is guidance on how your medical practice should code a preoperative routine physical exam, including when to use CPT codes 99241-99245 and 99251-99255.

To fee or not to fee?

What do payers know about medical necessity anyway? Reduce those annoying denials and collect what you deserve.

Insurance companies are adding functionality to their Web sites - like recredentialing and comprehensive claims management - to make working with them a little easier.

On average, 30 percent of all claims are denied - and half of those are never resubmitted. Is it time to put your billing process through the paces?