
Coding questions? We've got the answers.

Coding questions? We've got the answers.

Coding questions? We've got the answers

Understanding third-party payers can go a long way to making your life easier.

Defunct payment policies, denied claims, and unchallenged audits all blled revenue from practices. Here's what it means and how to stop it.

With the right technology, your practice can do a better job of collecting upfront copayments, catching likely claims denials, and tracking patterns.

Claims denials can hurt practice revenue, so stay on top of your billing process to collect every penny you've earned.

Coding questions? We've got the answers

Our latest analysis of the annual ranking of payers based on hassle factor is here. The good news: Most insurers are paying faster, denying less, and making their processes more transparent. But there's still room for improvement.

To stay safe and weed out the billing and collections problems stifling your practice's revenue stream, our experts recommend a "bottom-to-top" assessment of your entire billing operation.

The Affordable Care Act added a new Medicare Annual Wellness Visit. Contrary to patient and physician expectations, it is not a physical exam.

Why spend hours on the phone with payers when you can check online in minutes?

Coding for observation services can be confounding. Currently, CPT and CMS disagree on which code to report on the second day of observation. In 2011, that is changing.

What can you do if your payer won't reimburse your practice for cleanly submitted claims?

Here’s how to use these code add-ons correctly to help you get paid what you deserve

One of the thorniest coding questions is: Can a physician bill for family meetings when the patient is not present? If so, who gets the bill ?

Advance preparation is your key to successfully managing the ICD-10 conversion. Here’s what your practice needs to know and do to get ready.

If you can't verify a patient's insurance, their signature on this form shows they know they are responsible for payment.

Medicare denies claims for 26 percent of all services submitted. More distressing -- 40 percent of those services are never resubmitted for payment by providers. Talk about missed opportunities! Customize this form letter -- and the ones below -- to appeal claims denied, no matter who the payer is. Use this letter to show payers that the claims you are sending are not dups, but corrections.

Compare your denial rate from Medicare to national averages for your specialty by total amount denied, number of services denied, or percent of services denied. Data from the Centers for Medicare and Medicaid Services.

Manage your denials from insurance companies by tracking them in this worksheet. Track the denials according to the functional area to identify opportunities for improvement. By tracking and monitoring denials, you can fix the problem and prevent denials in the first place.

Specialists, use this waiver if a patient forgot his referral. It says that the patient agrees to pay for services rendered that are not covered by his managed care company.
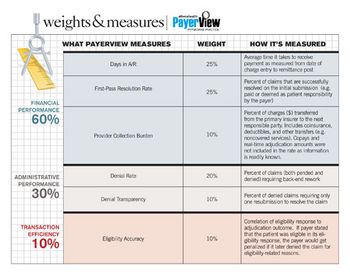
Our fifth edition of PayerView uses real claims data to examine and rank payers based on financial and administrative performance, as well as efficiency. Here’s to friendly competition that helps docs get paid.

What is the simplest method for reducing denials? Get the correct patient data from the start.

Medicare is getting more aggressive with audits through its Recovery Audit Contractor program. Here’s how to assess your billing procedures to avoid audits, and establish a process for when a RAC does come knocking.

Billing massage chair use; using the AI modifier; getting paid for pulse ox.