
Since 2011, only one in every two or three physicians has attested to the Stage 1 rules of meaningful use. Why should this matter to your practice?

After a 15-month fight with Long COVID, author Lucien W. Roberts, III, MHA, FACMPE, retired in February 2022 on the advice of his primary care doctor and his wife…perhaps not in that order.In retirement, he spends a few hours a week at a freestanding infusion center he co-owns, writes the occasional article, and tries not to drive his wife too crazy.He may be reached at lroberts@theinfusionsolution.com.

Since 2011, only one in every two or three physicians has attested to the Stage 1 rules of meaningful use. Why should this matter to your practice?

The best defense is a good offense. Arm yourself with knowledge on what new federal healthcare fraud and abuse measures mean for your practice.

While many practices have a compliance plan, most sit on a shelf gathering dust. Take it down, dust it off, and read it. Unenforced, it could be your worst enemy.

Don't let your patients judge you by the dusty philodendron sitting in the corner. Use our easy checklist to make sure your waiting room measures up.

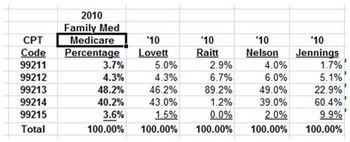
Don't let your practice be caught up in Medicare's recovery program. It's a simple matter to examine your own coding patterns and compare them to national utilization data.

By empowering your staff, you can improve the performance, care, and service your practice provides. Some call the concept employee empowerment, others call it employee engagement; I call it common sense.
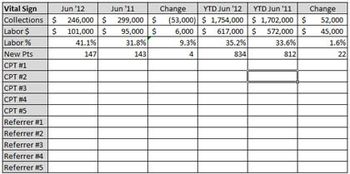
Most physicians have a limited amount of time to monitor the fiscal health of their practices. However, it is possible. Here are five quick measures to make the task easier.

There is much more to billing than just billing; make sure your practice is getting it right.

Here's how your medical practice should build a plan for the looming transition from ICD-9 to ICD-10 in 2014.

9 steps to creating and preserving your patient pipeline

Because all medical practices are impacted by Medicare cuts ―as most payers tie their fee schedules to Medicare ― it is incumbent upon each of us to step up and make our voice heard.

Walgreen's, Target, and other retail outlets are selling flu shots, physicals, and an ever expanding list of minor healthcare services traditionally provided in physician offices.

Here's my prediction: your practice will be audited in the next 24 months and asked to return overpayments.

Knowing what a triple net is ― and isn't ― will help practices understand the true costs of their office leases.

In medicine, there is an important distinction between clinical quality and perceived clinical quality. They are rarely one and the same, and understanding this distinction is critical for both clinicians and practice administrators.

The feds have aggressively stepped up their fraud and abuse efforts. Your practice may play by the rules, but that doesn't guarantee it will escape federal scrutiny.

ACOs will come in many shapes and sizes; until the final rules are announced, here are eleven things you should know.

You might feel more justified than most in taking out your frustration on others, but be careful - the emotional hangovers you might create can often have a long-lasting effect on your practice.

Inflation can be both good and bad for a practice. Therefore, understanding the nature of inflation can save your practice money.

The deadline for conversion from the present electronic claims transaction standard to Version 5010 is fast approaching. Make sure both your practice and systems vendor are ready for the change.

Medical practices face two significant deadlines that require planning and testing in 2011. The first is the new 5010 electronic claims transmission standard, the second ICD-10.

I avoid most e-mail offers trying to sell me something; don't need the superfluous e-mails cluttering up my inbox.

There are many intangibles to consider before sitting at the table with a payer to negotiate reimbursement.

One thing that creates friction in medical practices is the success and subsequent recognition of one of its members.