
Answers from our coding expert on questions regarding the Medicare Annual Wellness Visit; urea breath tests; counseling time; and consultations.

Answers from our coding expert on questions regarding the Medicare Annual Wellness Visit; urea breath tests; counseling time; and consultations.

The incident-to rules can be confusing for many physicians, practice managers, and billers and coders. Here's some helpful guidance.

The results of our 2014 Fee Schedule Survey are in. Here's a look at some of the key findings, and how physician practices can react.

Test your patient collections knowledge with our interactive quiz, featuring claims and denial data from RemitDATA from the fourth quarter of 2014.

Over the summer CMS added four new modifiers that will require a much greater degree of specification when coding surgical procedures.

In early 2015, your first tasks to prepare for ICD-10 should be reviewing your budget and effectively communicating the code set change.

Now is the time to act to prevent claims issues, including denials, due to ICD-10. Here are four tips.

The ICD-10 deadline is only nine months away. Here are six questions to ask your software vendors immediately.

Q: When a patient has been admitted and discharged on the same day, can one note support a same day admit/discharge code?
Our experts at Physicians Practice Pearls have written on a wide variety of practice-management topics, but these eight columns stood out as the gems.

With the ICD-10 transition on the horizon, medical practices need to start preparing. Here are three tips to start with when the calendar flips to 2015.
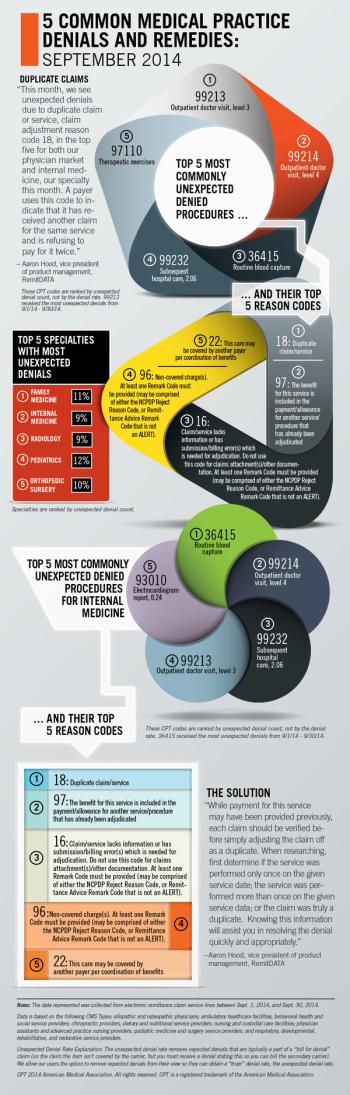
RemitDATA's Aaron Hood explores the most common unexpected denials at practices nationwide, with a special focus on internal medicine.


Our practice does internal chart reviews on our physicians for coding accuracy. What do you feel is an appropriate passing score?
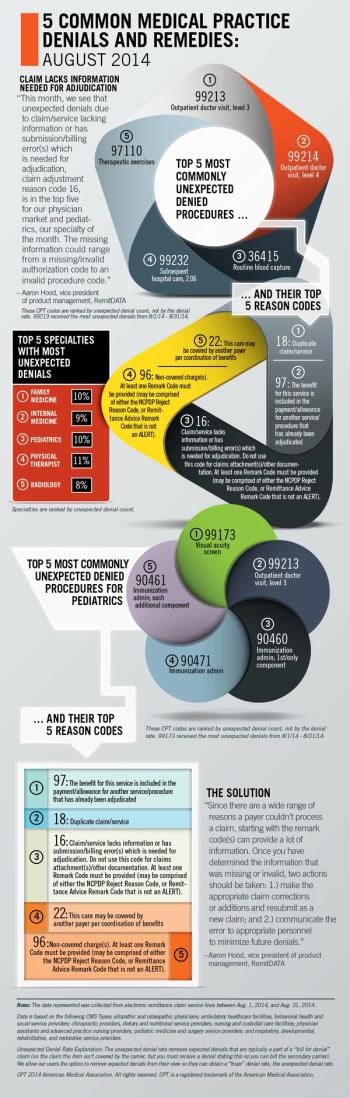
RemitDATA's Aaron Hood explores the most common unexpected denials at practices nationwide, with a special focus on pediatrics.

A change by CMS to its claims submission process for Medicare Advantage affects both physicians and their practices. Here's what you need to know.

To truly be ready for the ICD-10 transition, start your communications now: with your physicians, your staff, and your tech vendors.

Get coding guidance on billing for a family medicine group; patients being seen at a new practice; and more.

Reporting vaccine administration can be tricky. Practices should review most recent updates and be aware of differences between commercial and federal payers.
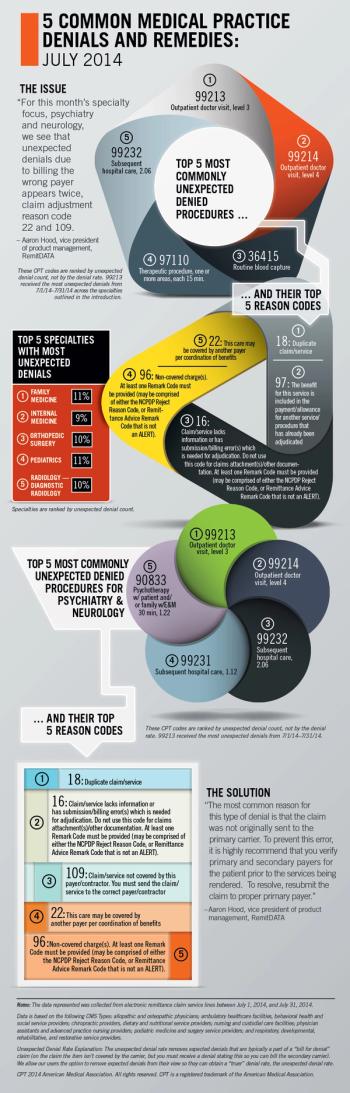
RemitDATA's Aaron Hood explores the most common unexpected denials at practices nationwide, with a special focus on psychiatry and neurology.

Get coding guidance on resident consultation via telephone; discharging patients; antepartum care; and more.

Not only should your practice prepare to use new modifiers by Jan. 1, you might also experience even greater scrutiny of future modifier 59 claims.
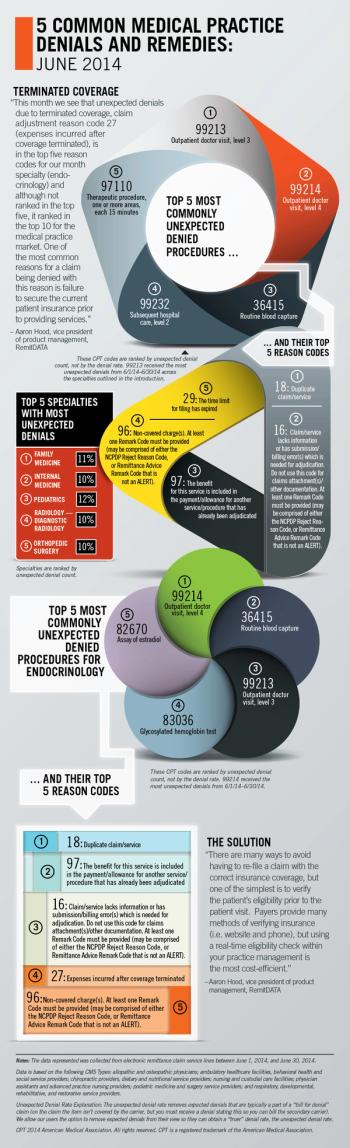
RemitDATA's vice president of product management, Aaron Hood, explores the most common unexpected denials at practices nationwide, focusing on endocrinology.

Reviewing the definitions of modifiers first will ensure that applying a modifier goes from a game of chance to a sure thing.

Performing an audit on your denials will provide a clear picture of where you need to focus your attention in the billing process.