
Physicians are first concerned with treating patients. But they are also business owners. It is a mistake not to review potential areas of risk.

Physicians are first concerned with treating patients. But they are also business owners. It is a mistake not to review potential areas of risk.
What are the rules when it comes to completing chart notes after the time of service? Can doctors charge a copay for an annual exam?

It's been one year since ICD-10 has come into effect. How did practices deal with the transition and what's next?

CPT designates six codes to report vaccine administration. Here's how to make sure you are reporting the correct service and conditions.
While the ICD-10 grace period was relevant to only CMS, there is still work to be done. Here are nine steps practices can take to ensure post Oct. 1, they are ready.

This month's coding questions tackle whether physicians in the same group practice in the same specialty have to bill as a single doctor.

In the world of coding, here's why an attending physician is not really allowed to attest to an NP consult. Also, what are comparative billing reports?

Can you code when a patient is so distraught an appropriate history cannot be obtained, nor can a mental status exam be performed?

How to institute vaccine administration codes for patients who are older than 19 years of age. Also, guidance on follow-up codes in electronic billing.

Coding for TCM services should include global periods; dates of service; and correct documentation.

TCM helps patients transition from the hospital to the community. Many physicians, however, miss deserved reimbursement because they lack documentation.

Patients can understand so little about their health plan that the billing department is automatically blamed when something goes wrong.
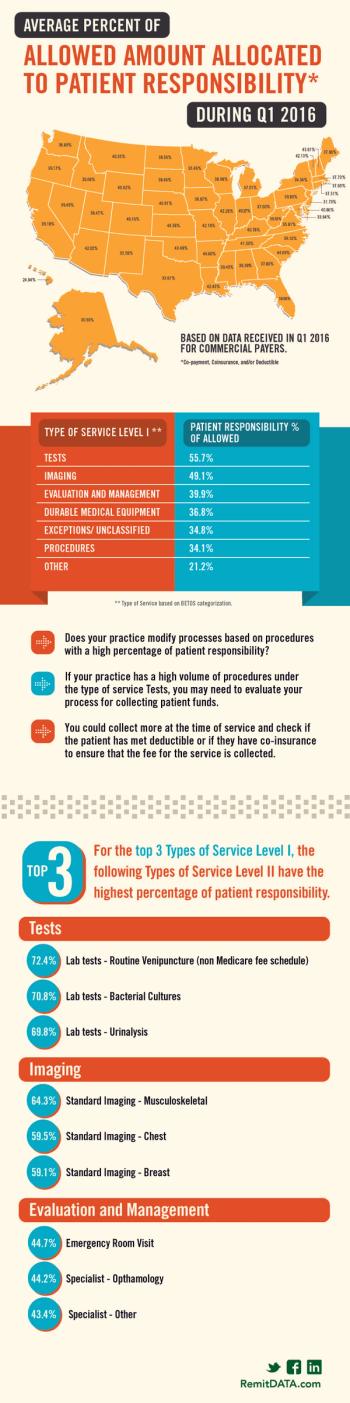
What state allows for almost 50 percent patient responsibility? Also, which services have the highest percentage of patient responsibility?
Physicians who spend significant time coordinating a patient's care may realize reimbursement in several ways.

Our coding expert discusses what to do when Medicare denies a consult code; preparation for Medicare chart audits; and coding for unusual services.

Here's why you should ignore "Incident to" Billing for PA services, which require a significant amount of additional work without a fair return in revenue.

Answers from our coding expert on questions regarding advance care planning; pessary cleaning; and identifying inclusive codes.

While some payer-based investigations into fraud might be based on actual patterns of abuse, most are just an attempt to recoup funds.

Was the fear and trepidation surrounding ICD-10 overstated or is the early success around a lack of denials only temporary for providers?


When you look at your cash inflow each month, are you disappointed? That's why it is so important to identify why your claims are being denied.

Proper documentation and reporting of codes for prolonged services allows providers to improve compensation for lengthy outpatient services.

Since the implementation of the ICD-10 coding system, most claims are processing smoothly and rejection rates have been minimal.

Answers from our coding expert on questions regarding incident-to billing; time-based coding; and specificity in ICD-10.

Answers from our coding expert on questions regarding medical necessity; using the ROS for history of presenting illness; and duplicative coding.