
E&M coding guidelines are finally changing after 20 years, but don't celebrate yet. These changes may be worrisome to practices

E&M coding guidelines are finally changing after 20 years, but don't celebrate yet. These changes may be worrisome to practices
Take this quiz from RemitDATA on the coding trends in the first half of 2017.

What happens when a patient presents with a condition that there is currently no billing code in the system for? This doctor finds out the hard way.

Coding expert Bill Dacey has some of the most recent updates to the coding manual. What do you have to know for 2018?
This doc found out the hard way that medical coding for a single patient can be a cumbersome time suck.

Should you hire an in-house coder or outsource? Do you need to hire one at all? Answers to these questions and more.

Physicians need to document care in the EHR, but they can either keep the computer out of the room or embrace it to focus on the patient.
The coding rulebook is always changing. Here are strategies from our two coding experts to help you stay compliant.
Inaccurate billing and coding can have a direct and negative impact on a practice's bottom line. What are some common coding queries?
Experts share their advice on how to ensure coding is done properly at your practice, through focusing on common codes and more.

Coding expert Bill Dacey answers your latest coding questions, including an inquiry on how to bill for TCM services.

This month's coding questions tackle depression screens on elderly patients and coding for interactive complexity.

Using telehealth services? Here are the basics on reporting this to Medicare, in order to get properly paid.

In this month's coding column, we also feature answers to prolonged services codes and orthopedic ICD-10 codes.

Everything you want to know about coding a transitional care management encounter, including what services are included.

With medicine's increased demands and time constraints, doctors are less likely to practice the healthy lifestyle they preach to patients.

For this month's coding column, we get a few ICD-10 specific questions on BMI and well child visits.
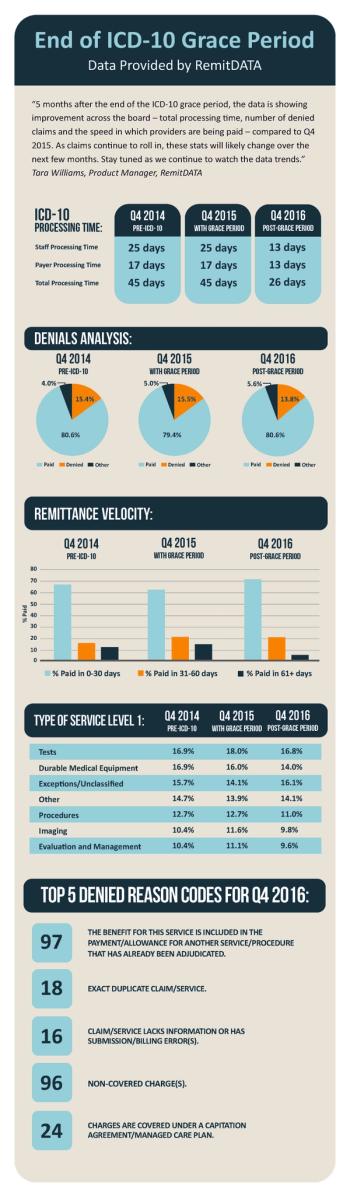
A new infographic from RemitDATA reveals practices have seen improvements in processing speed, denials, and more since the end of the ICD-10 grace period.

This month's coding column: What do physicians have to know about coding for telemedicine visits?
In honor of March Madness, we asked our editorial advisory board to tell us which sports they loved to watch on TV.

This month's coding column: An elderly patient's grown daughter comes in for an office visit without the patient, is there a code for that?

Revised codes and coding guidelines for 2017 completely change reporting for moderate sedation services. Here's what you have to know.

The 2016 Physicians Practice Fee Schedule Survey reveals how much more employed docs get paid than independent physicians for certain CPT codes.
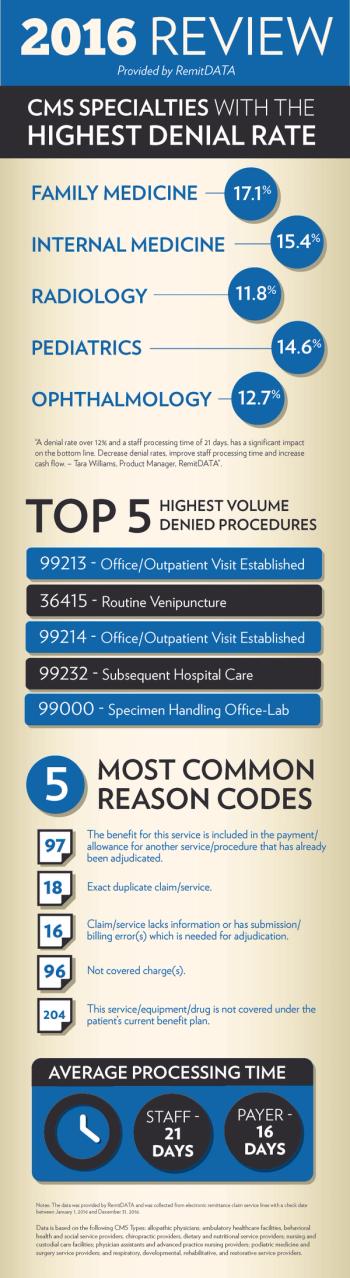
A new infographic from RemitDATA reveals which five specialties and five procedures had the highest denial rate in 2016, as well as the five most common reasons why.
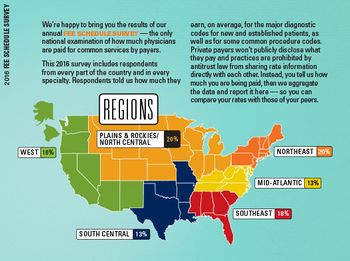
What do practices get paid for common codes? The results to the 2016 Fee Schedule Survey, featuring more than 1,100 respondents from across the country, provide the answers.