
Can you code when a patient is so distraught an appropriate history cannot be obtained, nor can a mental status exam be performed?

Can you code when a patient is so distraught an appropriate history cannot be obtained, nor can a mental status exam be performed?

If your practice is struggling to collect all that it is due from patients, here's how you can stack the deck in your favor.
When using third-party vendors for certain practice functions, it's always wise to take a close look at their performance.
Buying medical equipment for your practice that must be replaced every few years may not be the best way to go. Here's what you should know about leasing.

Good customer service is a hallmark of the successful practice. Don't let third-party vendors give you a black eye.

How to institute vaccine administration codes for patients who are older than 19 years of age. Also, guidance on follow-up codes in electronic billing.

Coding for TCM services should include global periods; dates of service; and correct documentation.

TCM helps patients transition from the hospital to the community. Many physicians, however, miss deserved reimbursement because they lack documentation.

Patient can be irate when it comes to higher than expected bills. This practice found the best way to address the issue is to be frank.

How can administrators bring together physicians, advanced practitioners, and nurses, and create a culture of collaboration?


Patients can understand so little about their health plan that the billing department is automatically blamed when something goes wrong.
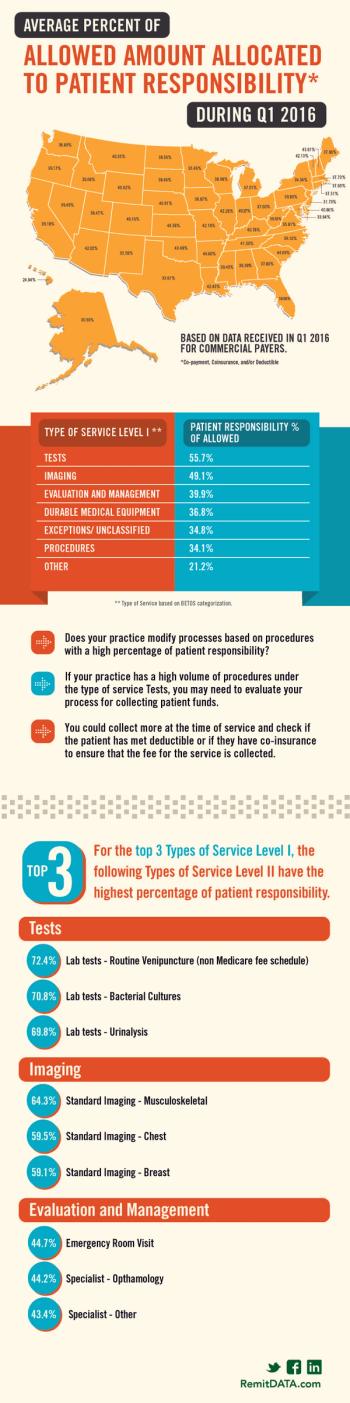
What state allows for almost 50 percent patient responsibility? Also, which services have the highest percentage of patient responsibility?

Practices need to expand their leadership capabilities beyond clinical-minded decisions. They have to focus on business management, too.

Vendors' products and services directly impact a practice's day-to-day operations. Here's how to be establish efficient vendor relations.

Spending a few minutes explaining health insurance benefits to patients prior to the appointment should become a requirement.

Physicians are frustrated with the lack of clear specifics on how they will meet quality metrics to avoid a negative payment adjustment in 2019.

This doctor says one patient's care plan reemphasized why he has continued to stay independent in the era of consolidation.
Physicians who spend significant time coordinating a patient's care may realize reimbursement in several ways.

Because the replacement for Medicare's SGR is complex and potentially difficult to participate in, physicians must arm themselves with knowledge.

A good vendor does more than just submit claims and hope for the best. Here are eight things you should expect from your medical billing service.

When you read reviews on online review sites, you typically read about the physician. But have you ever read how awesome the billing experience was?

Our coding expert discusses what to do when Medicare denies a consult code; preparation for Medicare chart audits; and coding for unusual services.

Doctors are dealing with more outside forces than ever before, like third-party and government payers. Here's why they have to organize.
It's not impossible. Smaller providers can maximize their RCM and increase their bottom line; here are seven ways to do just that.