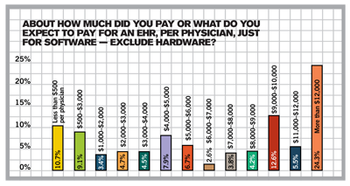
If you’re confused about the federal incentives to buy an EHR and what meaningful use means, you're not alone. We have the answers in our 2010 Technology Survey.
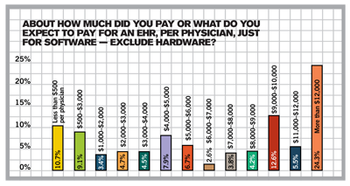
If you’re confused about the federal incentives to buy an EHR and what meaningful use means, you're not alone. We have the answers in our 2010 Technology Survey.

Advance preparation is your key to successfully managing the ICD-10 conversion. Here’s what your practice needs to know and do to get ready.

Here’s how to skip the drama and hire right the next time at your medical practice.
Patients must be educated about the purpose of the medical home and the need for care coordination.
As more doctors go to work for hospitals, more of their colleagues are thinking about giving up private practice. But is this the only way to go-and will it help fix the healthcare mess or make it worse?

If you can't verify a patient's insurance, their signature on this form shows they know they are responsible for payment.

CMS has released its proposed changes. Not sure how it will impact you? Have a gander at this. It'll give you what you need to prepare. We took it straight from the horse's mouth, straight from the proposed regulations.

Follow our flowchart to find ways to improve your collections. A great companion to our Accounts Receivable Key Indicators calculator. If your results there are lower than you like, this flowchart will help you improve.

Medicare denies claims for 26 percent of all services submitted. More distressing -- 40 percent of those services are never resubmitted for payment by providers. Talk about missed opportunities! Customize this form letter -- and the ones below -- to appeal claims denied, no matter who the payer is. Use this letter to show payers that the claims you are sending are not dups, but corrections.

This is similar to the general notice above, but is specifically for laboratory work. Again, this form comes directly from the Center for Medicare and Medicaid Services. Access its Web site for more information.

Compare your denial rate from Medicare to national averages for your specialty by total amount denied, number of services denied, or percent of services denied. Data from the Centers for Medicare and Medicaid Services.

Manage your denials from insurance companies by tracking them in this worksheet. Track the denials according to the functional area to identify opportunities for improvement. By tracking and monitoring denials, you can fix the problem and prevent denials in the first place.

This simple work sheet will let you compare your payers' reimbursement for specific procedure with your costs for each procedure. If you're spending more to provide a service than you're making for it, then it's time to address the problem.

Use this easy calculator to find out which of your payers are worth your efforts. By comparing the percentage of revenue to the percentage of patient encounters for each of your payers, you can tell at a glance which plans are the poor performers.

Physicians often want to review an overdue patient account before it is sent to a collection agency. Staff can use this form to summarize the status of the account, making review easier.

Opening a new practice? Here are some of the things you will need to get done before the doors open.

Use this sample template for guidelines on documenting patient visits in general. Provided by Hill & Associates.

Plain language advice on using common modifiers in your medical coding.

Take a page from your mortgage company. Instead of sending self-pay patients on a payment plan statements every month, give them coupons.

This is the first in a series of letters to use for patient collections.

Use this sample template for guidelines on documenting established patient visits. Provided by Hill & Associates.

Let new patients know about your policies from the get go. Follow these guidelines.

Specialists, use this waiver if a patient forgot his referral. It says that the patient agrees to pay for services rendered that are not covered by his managed care company.

Use this sample template for guidelines on documenting outpatient visits. Provided by Hill & Associates.
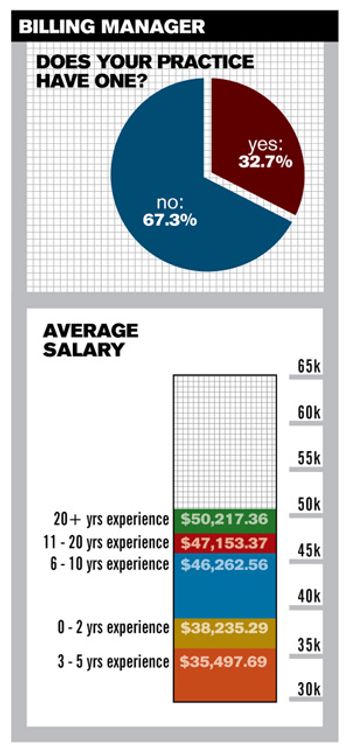
It’s hard to know how much is enough when it comes to recruiting and paying staff. Wouldn’t it be great if you knew what everyone else was paying their staff and could compare? Now you can. Our staff salary survey returns for a second year of national and regional salary stats, plus expert advice from seasoned veterans.