
With prices low, it may seem like a great time to buy your office space. Be wary; the advantages to ownership, while real, are balanced with disadvantages and risk. Make sure your eyes are open.

With prices low, it may seem like a great time to buy your office space. Be wary; the advantages to ownership, while real, are balanced with disadvantages and risk. Make sure your eyes are open.

EHR companies are increasingly offering billing services, and vice versa. Is this just another way to squeeze money out of you, or does it make sense to combine the services?

Here's how to properly use E&M code 99213, including when other CPT options might be more appropriate with patients at your medical practice.

The traditional practice of primary care is complex - let’s face it, you could more accurately predict the likelihood of a patient presenting with a subdural hematoma based on his or her symptoms than you might Blue Cross’ likelihood of accepting a preauthorization for the CT scan.

Say goodbye to photocopies: Machine-readable cards could make billing and collections easier. When will payers make them widely available?

Medicare hopes to save millions with tougher billing rules and aggressive audits - changes that could cost your practice money. But if you bill right and on time, you can keep that Medicare check coming.
Which payers should you deal with and which should you drop? PayerView uses real claims data to rank them first to worst.

Billing “Incident-To;” Same Patient, New Problem; Moonlight Coding

Assignment of Benefits

Appeal letter for prompt payment from your medical practice payers.

Here is a sample collections letter to use at your medical practice.

Collections Letter 3

Collections Letter 3 -- Spanish

Collections Letter 2 -- Spanish

Appeal Letter Justifying Emergency Treatment

Collections Letter 1 -- Spanish

If you can't verify a patient's insurance, their signature on this form shows they know they are responsible for payment.

Appeal Letter Justifying Medical Neccessity

Assignment of Benefits -- Spanish

Use this letter when a claim is denied because a patient saw a physician in your group who is not his or her designated primary care physician.

This Advance Beneficiary Notice form, created by CMS, is best managed by the clinical team at your medical practice versus the front office staff.

Use this letter if a patient consistently refuses to pay for services rendered, and you are forced to dismiss the patient from your practice.

Outsourcing billing operations can be a relief to a frazzled practice. But you need to do it right; after all, your practice’s revenue is at stake.
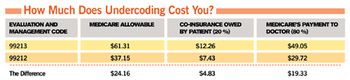
Coding is no fun, but you gotta get it right if you wanna get paid. Here’s our guide to coding like a pro.

This time, it's back with a quality twist.