
Yes, there is a way to make more money; by providing better care - and you needn’t wait for some P4P program or “medical home��” experiment to get started.

Yes, there is a way to make more money; by providing better care - and you needn’t wait for some P4P program or “medical home��” experiment to get started.

The results of our annual fee schedule survey tell you how much to expect from payers. The news isn’t good, but we have plenty of advice for making the most of difficult times.

You’ve heard it all from patients who have outstanding accounts. How can you tell a genuine plea for help from a sob story, and when does it matter?
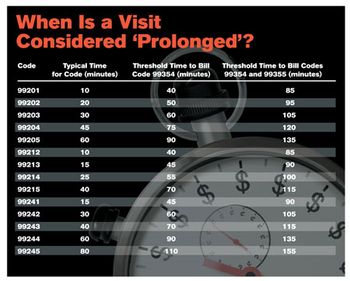
Attorneys bill for their time - don’t you wish you could? What if we told you that you can? Here’s how.

It’s time to get those annual coding upgrades to your billing software. But, how can you defray the cost without losing the upgrades?

Forms for summer camps, sports teams, and schools - all require you to take uncompensated time to fill them out. Here’s our primer on how to develop your own policy for getting paid fairly.

Should you outsource your practice’s billing, or keep it in-house? Revenue cycle management vendors promise to reduce denials, improve collections, and get you your money faster. But, are they for you?

High-deductible health plans like health savings accounts are becoming more common, and that means you’ll have to work harder to collect from patients.

Deborah Grider, CPC/EM, president of the American Academy of Professional Coders National Advisory Board talks about what you aren’t billing that is costing you big.

We go beyond Billing 101 to show you the advanced techniques and little-known secrets for collecting every nickel, dime, and Spanish doubloon you’re owed.
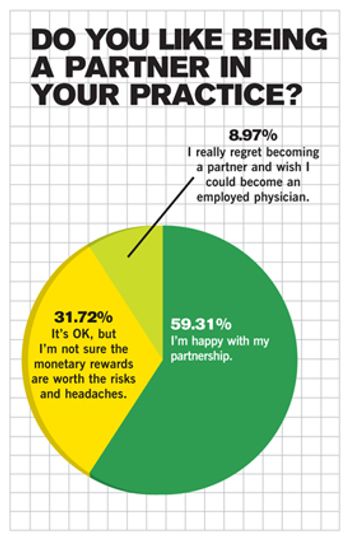
There’s encouraging news in our third annual Physician Compensation Survey. Primary-care docs are seeing their incomes tick upward - on average. Where do you stack up?

Thinking of keeping your billing process in-house to save money? OK, but be sure you really are saving money in the long run.

In America’s Chocolate City, a diminutive practice administrator takes on the big payers, and gets results.

The government rocked the hospital world with its plan to stop paying hospitals for the treatment necessary to fix their so-called mistakes. Could your office be next?

Collecting from patients is one of your hardest jobs. Some practices, in frustration, are turning to tough tactics like charging interest and even taking patients to court. Here’s a look at what works best, and what’s not worth the trouble.

Our new occasional series on the nexus of healthcare and the changing economy begins with a look at health savings accounts. Increasingly popular with patients, HSAs promise owners the chance to have more control over how their healthcare dollars are spent. Yet they present unique challenges for your billing office.

Here is guidance on when and how to use the GV and GW medical coding modifiers in hospice work for attending physicians.

The government has some ideas about what’s wrong with Medicaid, and how to fix it. Too bad their ideas don’t have much to do with paying doctors better.
We hear you. Unfortunately, physician reimbursement continues to decline, according to the results of our exclusive 2007 Fee Schedule Survey. That’s the bad news. Now here’s the good news: Along with all the hard data, we arm you with the tools you need to fight back.

When asked to a see a patient by another physician, does it really matter if you bill an E&M visit as a consult or a referral? It sure does - and using these terms interchangeably can cost your practice thousands. We help sort out the differences.

You deserve every penny you’ve earned. But if your practice is like most, you probably aren’t getting that. There are technologies out there that can help - but which one is right for you?

Your days-in-A/R report tells you how long it takes you to get paid - and the longer it takes, the more it costs. Learn how to read these reports correctly so you can fix whatever’s holding up your checks.

A Texas psychiatry practice gets help finding its backbone in dealing with negligent payers.

Patients are increasingly asking doctors to keep diagnoses and treatments out of their records to avoid damaging their chances of obtaining insurance coverage in the future. What should you do?

Tired of being judged by payers? Here’s your chance to turn the tables and judge them. With help from our friends at athenahealth, we give you the second annual PayerView rankings. It’s a report card that uses real claims data to judge dozens of local and national payers on how well they treat you, the physician. Compare this data with your own; then strive to change what isn’t working.