
CPT designates six codes to report vaccine administration. Here's how to make sure you are reporting the correct service and conditions.

CPT designates six codes to report vaccine administration. Here's how to make sure you are reporting the correct service and conditions.
While the ICD-10 grace period was relevant to only CMS, there is still work to be done. Here are nine steps practices can take to ensure post Oct. 1, they are ready.

This month's coding questions tackle whether physicians in the same group practice in the same specialty have to bill as a single doctor.

There are four payment technologies to put on your radar as you prioritize plans for upgrades or the installation of new technology. [Sponsored]

Can you code when a patient is so distraught an appropriate history cannot be obtained, nor can a mental status exam be performed?

If your practice is struggling to collect all that it is due from patients, here's how you can stack the deck in your favor.
When using third-party vendors for certain practice functions, it's always wise to take a close look at their performance.

Good customer service is a hallmark of the successful practice. Don't let third-party vendors give you a black eye.

How to institute vaccine administration codes for patients who are older than 19 years of age. Also, guidance on follow-up codes in electronic billing.

Coding for TCM services should include global periods; dates of service; and correct documentation.

TCM helps patients transition from the hospital to the community. Many physicians, however, miss deserved reimbursement because they lack documentation.

Patient can be irate when it comes to higher than expected bills. This practice found the best way to address the issue is to be frank.

Patients can understand so little about their health plan that the billing department is automatically blamed when something goes wrong.
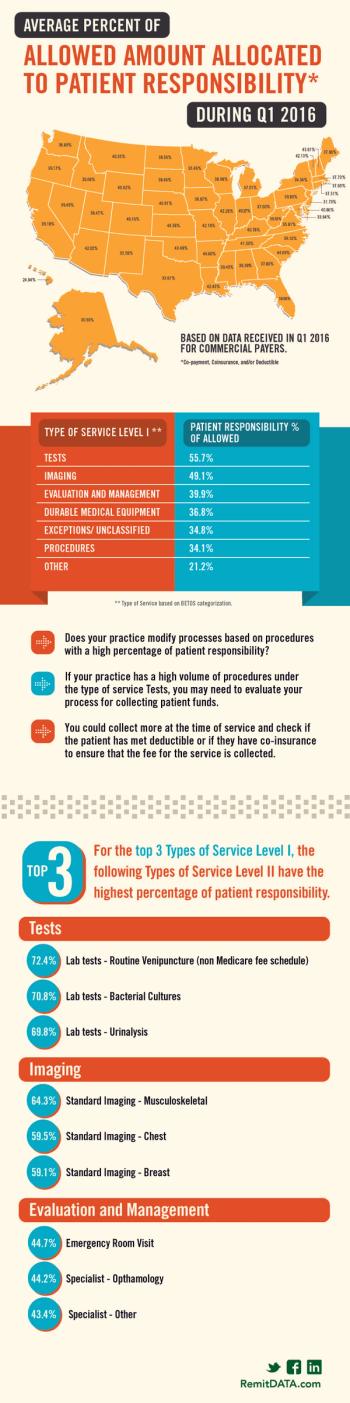
What state allows for almost 50 percent patient responsibility? Also, which services have the highest percentage of patient responsibility?

Spending a few minutes explaining health insurance benefits to patients prior to the appointment should become a requirement.

Physicians are frustrated with the lack of clear specifics on how they will meet quality metrics to avoid a negative payment adjustment in 2019.
Physicians who spend significant time coordinating a patient's care may realize reimbursement in several ways.

A good vendor does more than just submit claims and hope for the best. Here are eight things you should expect from your medical billing service.

When you read reviews on online review sites, you typically read about the physician. But have you ever read how awesome the billing experience was?

Our coding expert discusses what to do when Medicare denies a consult code; preparation for Medicare chart audits; and coding for unusual services.
It's not impossible. Smaller providers can maximize their RCM and increase their bottom line; here are seven ways to do just that.

In the second of a two-part interview with a CMS representative, more on the legal ramifications for waiving copays for low-income patients.

Most practices know they are obligated to collect patient copays and deductibles, but few know that for certain low-income patients doing so is illegal.
Government and commercial insurers have different policies practices must know about waiving copayments. What do practices have to know?

Here's why you should ignore "Incident to" Billing for PA services, which require a significant amount of additional work without a fair return in revenue.