
While recent concessions made by CMS on the ICD-10 transition may relieve stress for practices making the transition, some say it’s not enough.

While recent concessions made by CMS on the ICD-10 transition may relieve stress for practices making the transition, some say it’s not enough.
It makes good business sense to outsource the billing for most medical practices. That said, the outsourcing must be to a competent billing service.

By reviewing your fee schedule and comparing it to accounts receivable, you may find hidden money that you didn't know about.

Incomplete or inaccurate patient information can set the stage for a claim denial before a visit. Avoid these mistakes at the front desk.

Lack of feedback from back to front office on coding issues perpetuates a cycle of denials. Here are five tips to help get claims paid the first time.

A change in coding for behavioral screenings illustrates how payer payment policies negate any big-data promises of ICD-10.

Sometimes, you have to add a little muscle to the way your staff approaches patient payments and other collections for your medical practice.

If you believe billing processes need improvement in your practice, start by looking at the component steps of each task.

Superbills and other forms at your practice should also be prepared for Oct. 1, 2015. Here's how to get ready.

Our coding expert discusses coding for unspecified diagnosis at the time of encounter; a problem-focused exam; and scribe services.
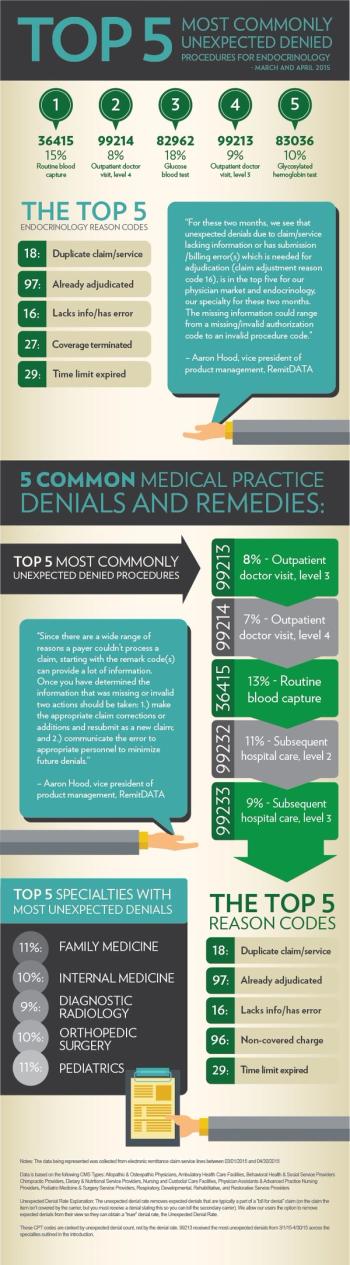
Get insight on the most common unexpected denials at practices nationwide, with a special focus on endocrinology, from RemitDATA.

ICD-10 Charts is a free tool to aid the coding transition, but also a gift from a son to his internist father to keep his private medical practice alive.

When it comes to complex payer rules, the most effective course of action is to consult experts for a thorough review of the rules and consequences.
Practices can often feel helpless when it comes to working with payers. Here's how they can change that dynamic and become empowered.

Many practices are running on razor-sharp margins. That puts them at a distinct disadvantage when it comes to dealing with payer-generated work.

Each year, athenahealth ranks payers on how easy they are to work with providers. Here are the top 20 in the "major payer" category for 2015.

Each year, athenahealth ranks payers on how easy they are to work with providers. Here are the top 20 in the "all payers" category for 2015.

Each year, athenahealth ranks payers on how easy they are to work with providers. Here are the top 20 in the Blues category for 2015.

Each year, athenahealth ranks payers on how easy they are to work with providers. Here are the top 20 in the Medicare category for 2015.

Each year, athenahealth ranks payers on how easy they are to work with providers. Here are the top 20 in the Medicaid category for 2015.

Make sure your practice is getting paid what it is owed for the work you perform with these four tips.

Available talent, specialty, and size are just three factors in deciding whether or not to outsource your practice's revenue cycle management.
Thinking about outsourcing your medical billing? Here are nine questions to ask a prospective outside biller or billing service.

Before deciding to provide and bill for chronic care management, a practice should make sure it has the necessary staff and support structures first.

As Oct. 1 approaches, get your physicians ready by determining how much and what kind of ICD-10 training they'll need.