Denials
Latest News
Latest Videos
Podcasts
CME Content
More News

Navigating payer denials requires the most expertise to handle within revenue cycle management
Recover revenue by utilizing proactive measures and technological solutions to navigate this difficult terrain.
Submission of incomplete or inaccurate claims results in claim denials, delayed payments, and additional work for staff. Here's how you can minimize claim denials and ensure timely payments for your practice.

Medical practices continue to be squeezed by increasing costs and decreasing reimbursement, emphasizing the need for better clinical coding and editing technology that can improve claims even before they’re submitted.

Adding appropriate technology to your practice can have profound effects on the well-being of your operations, allowing your workforce to focus on what they do best while you concentrate on patient care.
Denials are a painful - but preventable - financial drain on practices.

Ensure your practice’s long-term health by educating patients about their financial responsibility and staff on how to improve medical billing and collections.

Collecting patient payments can be a challenge for medical practices that aren’t operating at maximum efficiency. Review some key performance indicators to identify and improve processes.

A payer contract is more than a mere fee schedule. There are several other factors to consider when deciding to keep or terminate a payer contract.

Coding expert Bill Dacey answers your latest coding questions, including an inquiry on why Medicare denied an initial visit claim.

Practices sometimes can’t afford to administer treatment to patients given the risk of denied reimbursement claims.

Payers have made it so doctors cannot go with their instincts when caring for a patient and that's a shame.
The coding rulebook is always changing. Here are strategies from our two coding experts to help you stay compliant.
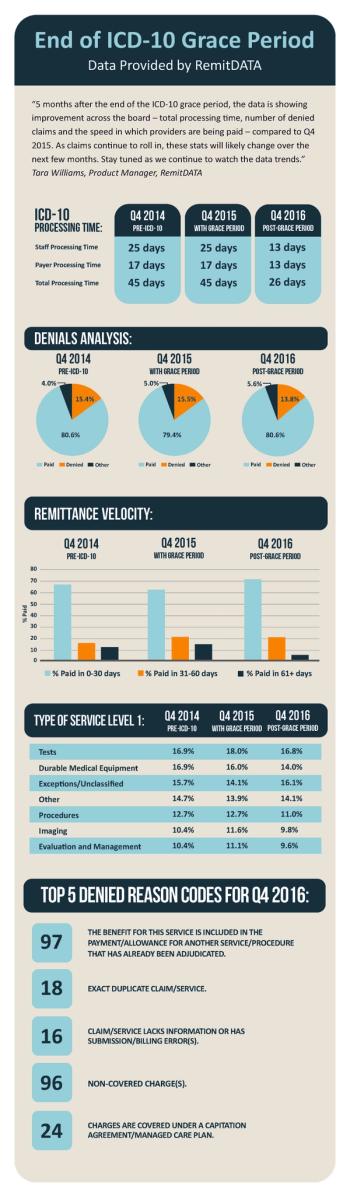
A new infographic from RemitDATA reveals practices have seen improvements in processing speed, denials, and more since the end of the ICD-10 grace period.
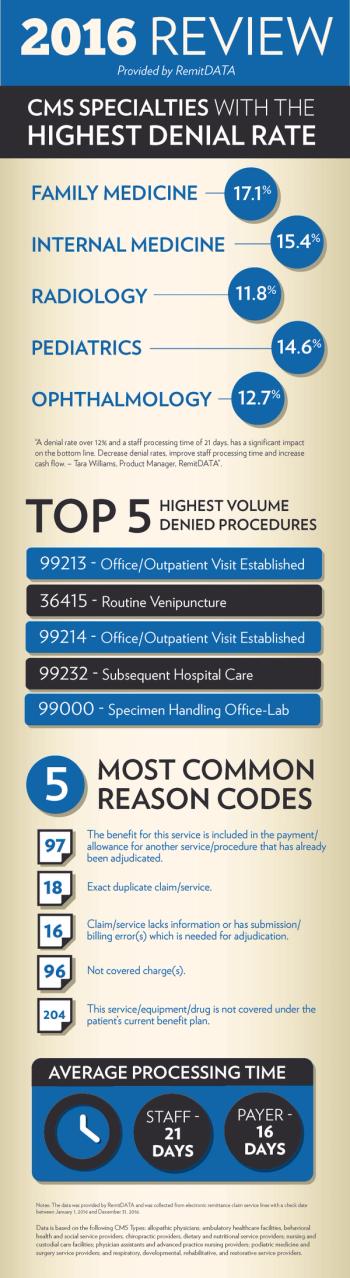
A new infographic from RemitDATA reveals which five specialties and five procedures had the highest denial rate in 2016, as well as the five most common reasons why.

This month's coding column looks at whether or not you can count addressing routine chronic conditions without a change in plan of care as E&M.
While the ICD-10 grace period was relevant to only CMS, there is still work to be done. Here are nine steps practices can take to ensure post Oct. 1, they are ready.

The retail pharmacy chain recently replaced an established drug with a replacement. It's a move that, in one doctor's opinion, usurps physician autonomy.

Two lawyers share a way that healthcare providers can challenge insurer recoupments in the ongoing struggle with payers relating to provider reimbursement.

This MD misses the day when the decisions in care were made by her - the doctor - and the patients. Today, the insurance company has a say.
During these early days of ICD-10 payers are accepting codes that aren't quite as specific as they should be. This won't last forever.

The early returns on ICD-10 from payers and a clearinghouse have been positive. Yet, no one is ready to pop the champagne and celebrate quite yet.

What were the top five most commonly unexpected procedures that were denied in August? RemitData laid out all the answers in this infographic.
Creating a game plan for dealing with an increase in denied claims during the first few months of ICD-10 can save you money and headaches.

Patients and payers are your two main practice revenue sources. Here's how to collect more for the work you do every day.