
Here are the tools available for the three main categories of document automation.

Here are the tools available for the three main categories of document automation.

Can multiple services from different providers be mixed or combined and billed together? Also, what are the rules for adding HCC codes at the end of your note?

Can provider types be mixed or combined and billed together? And does standard advice exist for determining telepsychiatry codes for various providers?

A generalized checklist for your planning.
How his experience contracting and recovering from the disease has shaped his perspective.

Remote visits and online E&M services.

Why has Medicare separated depression and alcohol screenings, and will patients incur cost-sharing with new patient portal E&M codes?
Documents required for Chronic Care management code 99490 and fulfilling the consult requirement.

Most audits concern outpatient visits.

CMS rules to simplify E/M coding and reemphasize patient narrative.


Practices are using E&M codes to bill for non-physician educational visits, but is this ok?
Submission of incomplete or inaccurate claims results in claim denials, delayed payments, and additional work for staff. Here's how you can minimize claim denials and ensure timely payments for your practice.

Existing medical documentation, particularly EHRs, needs to support physicians - not stymie them - as the industry transitions to value-based care.


Adding appropriate technology to your practice can have profound effects on the well-being of your operations, allowing your workforce to focus on what they do best while you concentrate on patient care.

Payers don’t dole out equal pay for equal work, so it benefits your physician practice to understand who pays what (so you can negotiate more).

Coding expert Bill Dacey clears up some confusion about split billing and combination visits.
“Probably one of the best decision's that I made, which has allowed me to continue to enjoy medical practice, was borne out of necessity.”

The ongoing battle to get patients the treatments they need is a major contributor to physician burnout.

If you don’t identify the coding issues, know that your potential buyer will.

Medicare’s new G2012 code for virtual check-ins may lead to cost savings. It could also cost patients money and potentially cost providers in patient satisfaction.
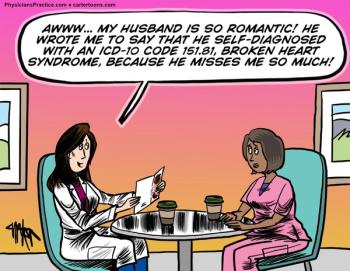
Don't worry. Romance is alive and well.

In order to justify the Level 4 E/M visit, make sure you have recorded all necessary information-and clearly label it for the payer auditor to easily find.

How to code varies on the circumstances. Many coding scenarios are determined by context-not absolutes.