
Payer requests for refunds for incorrectly processed claims are endemic. But wait! There are some things you can do before you write that check.

Payer requests for refunds for incorrectly processed claims are endemic. But wait! There are some things you can do before you write that check.

Say goodbye to photocopies: Machine-readable cards could make billing and collections easier. When will payers make them widely available?
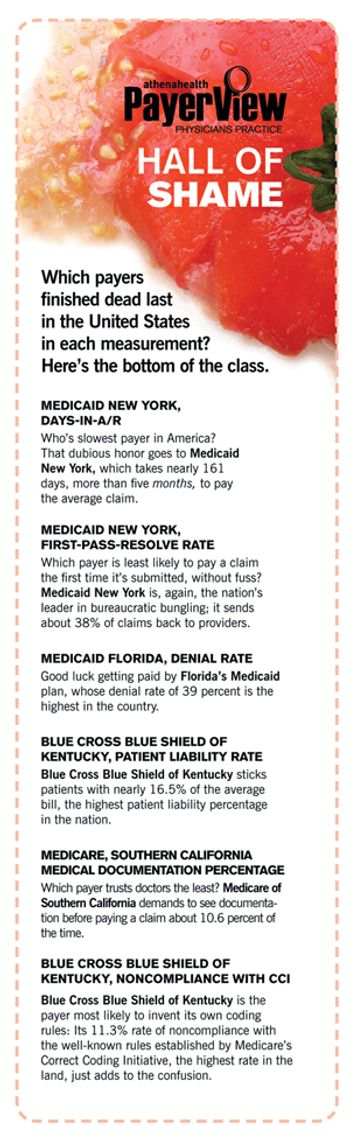
Which payers should you deal with and which should you drop? PayerView uses real claims data to rank them first to worst.

I just got a refund request from a payer. It’s for close to $1,000 for a patient we saw from 2004 to 2007. The payer now says the patient wasn’t eligible then. We checked, and it turns out the patient actually was on a Medicaid managed care plan and was not with the payer we billed. Still, Medicaid won’t consider claims from 2004. I just do not know what my options are. Are there any regulations to prevent this?

Could you please tell me how to negotiate higher reimbursements from commercial payers?

I started an urgent care clinic. The insurance companies will not recognize us even though I have gone through the expense to make the facility equal to a small ER. How do I get acceptance from the insurance companies?