
If you have been terminated by a provider, or notified you will be terminated, here's what you should know to know your recourse as a medical practice.

If you have been terminated by a provider, or notified you will be terminated, here's what you should know to know your recourse as a medical practice.
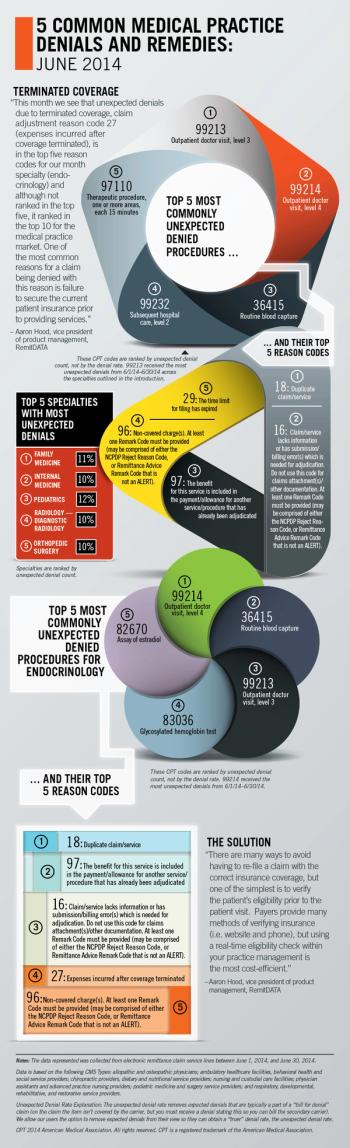
RemitDATA's vice president of product management, Aaron Hood, explores the most common unexpected denials at practices nationwide, focusing on endocrinology.

Small unpaid claims can add up to big problems for your medical practice. Here's how to find the best partner to collect what's owed for your medical services.

Here are two key areas where CMS could make adjustments to home health regulations that would benefit not just home health, but the industry in general.

Though more and more accountable care organizations are cropping up across the country, I don't believe they will be effective. Here's why.

Here are some strategies my medical practice has developed to get those unpaid patient balances off our books.

Quality of patient care is paramount, and I hope that the powers that be really think about realistic solutions to improving it.
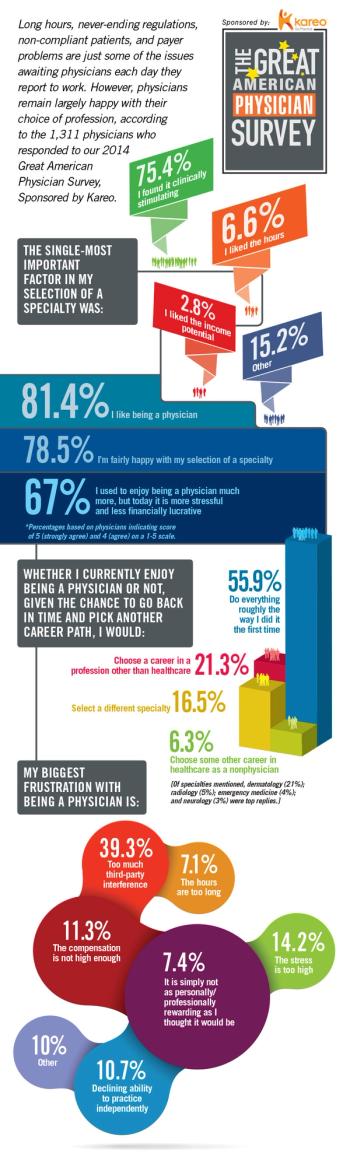
Our 2014 Great American Physician Survey, Sponsored by Kareo, indicates 8 in 10 physicians are happy as doctors and have no regrets about their career path.

Physicians have a multitude of options when structuring ACOs. Make sure you understand all the legal requirements before committing your practice.

With costs front and center for patients, in simple and stark terms: If you can’t deliver what the consumer perceives as quality, you will lose.

Done haphazardly or postponed until a month before a new physician starts, sloppy credentialing can spell cash-flow delays and more. Here's how to do it right.
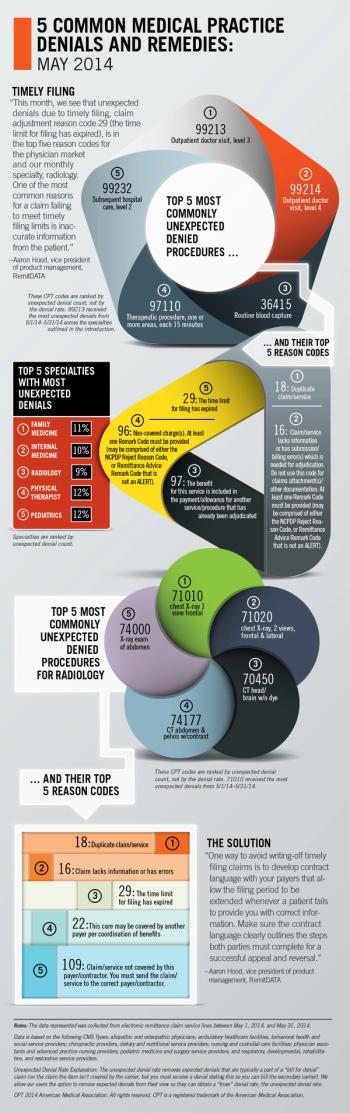
RemitDATA's vice president of product management, Aaron Hood, explores the most common unexpected denials at practices nationwide, with a focus on radiology.

Claims are paid based on the CPT code submitted to the payer. The diagnosis code supports medical necessity and tells the payer why the service was performed.

Hospitals are not only marking up and selling 340B-discounted drugs, but also buying up clinics to take advantage of the discount – a clear "progress trap."

The near future for physicians: Dying mom and pop store owners in a big-box health plan, hospital system world trading lab coats for a branded apron.

Payers can no longer exclude patients due to pre-existing conditions, so they are resorting to other tactics.

When patients refuse to pay their cost-share for healthcare, you have a surprise go-to resource to help get you paid.

When it comes to billing Medicare, you may very well be able to bill one physician incident-to another. Here's how.

When your patients have a great experience with your staff, but a not-so-great one with your billing department, it's time to make some changes.
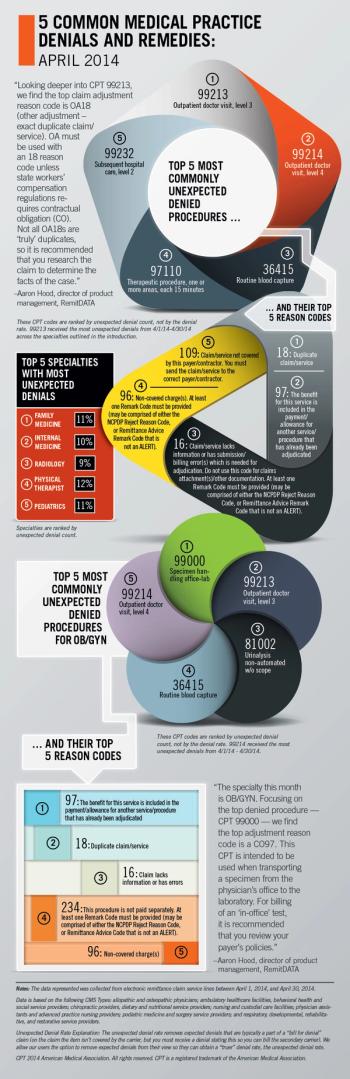
RemitDATA's director of product management, Aaron Hood, explores the most common unexpected denials at practices nationwide, with a focus on OB/GYN.

As part of its annual PayerView study, athenahealth outlines key areas where Medicaid is making business tough for physicians.

Each year, athenahealth ranks payers on how easy they are to work with providers. Here are the company's top 5 for categories including Blues, and regional.

Here are strategies for surviving a potential surge in patients with Medicaid and high-deductible exchange plans.

It hasn’t dawned on Washington that hospitals and hospital systems will never commit financial suicide by reducing volume, and physicians will pay the price.

The "recredentialing trap," strict payment reviews, and fingerprinting are all underway or on the horizon as ways payers are bullying physicians.