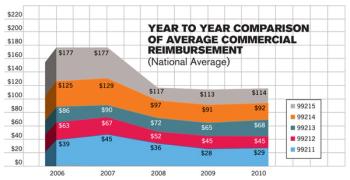
Changes with ICD-9 and CPT codes have been commonplace for several years and will almost assuredly continue, even with the adoption of ICD-10 in 2013. We must adapt to the change by updating our practice management systems to include the changes to ICD-9, CPT, and new rules by CMS and insurance payers.