
In 2014, the Affordable Care Act takes full effect. In 2015, penalties begin for not using EHRs. So perhaps now is the time to take a serious look at the technology.

In 2014, the Affordable Care Act takes full effect. In 2015, penalties begin for not using EHRs. So perhaps now is the time to take a serious look at the technology.

Addressing the privacy and safety concerns of mobile medicine should be as important as accessibility for today's medical providers.

Collaborations between physicians and other healthcare entities can be beneficial …but they can also violate federal and state antitrust laws.

Since 2011, only one in every two or three physicians has attested to the Stage 1 rules of meaningful use. Why should this matter to your practice?

What will the new HIPAA Omnibus Rule mean in terms of malpractice and professional liability insurance issues for physicians? Here's an explanation.

Two recent HIPAA violations, and a looming compliance date, mean now is the time to ensure privacy and security policies are in place at your medical practice.

Here's a primer on ERISA, how it works, and what it means for you and your medical practice.

HHS' Office of Inspector General reiterates antipathy towards some physician arrangements that carve out federal referrals.

Before joining a hospital or large health system, physicians should consider their potential partner's financing strategy.

Physicians considering changing their status as enrolled and participating Medicare providers must be aware of their options and legal requirements.
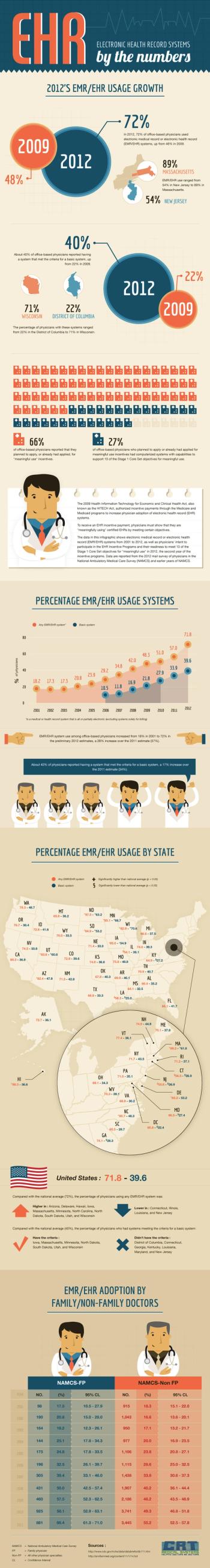
Here's a handy infographic on EHR adoption among private practice physicians, including data on certified EHR systems and meaningful use attestation.

The best way to approach all medical records in relation to HIPAA and the HITECH Act is the same as you do with patients: use universal precautions.

A Physicians Practice reader recently shared a dilemma he is facing in practice. Weigh in to help him best deal with this issue.

With health insurance exchanges on the horizon, some controlled by HHS, will federal laws fighting fraud and abuse have new teeth for physicians and practices?

Three recent examples show how being compliant and meeting medical necessity standards are the key to avoiding fraud enforcement actions.

How does the potential for drug diversion and addiction influence the way you care for patients with chronic pain?

Medicare and Medicaid providers must return overpayments once identified. Here are two different refund approaches for practices to consider when necessary.

Use of specialty-compounded drugs is on the rise, and so are associated risks for medical practices.

Here's an explanation of the rationale behind the Stark Law, the government's conflict of interest statute your medical practice needs to be aware of.

EHRs can indeed reduce costs and improve patient care, but they can also provide legal issues if the rules for their use are ignored.

What’s the best course of action when a patient threatens to sue you for malpractice?

Robert Anthony, a health specialist with CMS, explores key differences between Stage 1 and Stage 2 requirements for meaningful use in this webinar recorded June 4, 2013.

The federal government and private payers have declared war on physicians under the banner fraud, waste, and abuse. The AMA can't help, but you can take action.

A recent court case illustrates why physicians need to be vigilant in reporting incorrect claim submissions every time, all the time.

Opportunities to practice telemedicine are emerging due to improved technology and reimbursement. Still, there are some legal issues to consider.