
I have a 95 percent success rate when attempting to gain “approval” for medically needed testing. Here are some of my success strategies.

I have a 95 percent success rate when attempting to gain “approval” for medically needed testing. Here are some of my success strategies.

Not only should your practice prepare to use new modifiers by Jan. 1, you might also experience even greater scrutiny of future modifier 59 claims.

Charge capture has evolved, from paper to PC to PDA and now to mobile applications, providing physicians with better access to patient data.


Do you have a set policy for sending your delinquent patients to collections? By implementing a clear policy, you have a greater chance of collecting on those accounts.
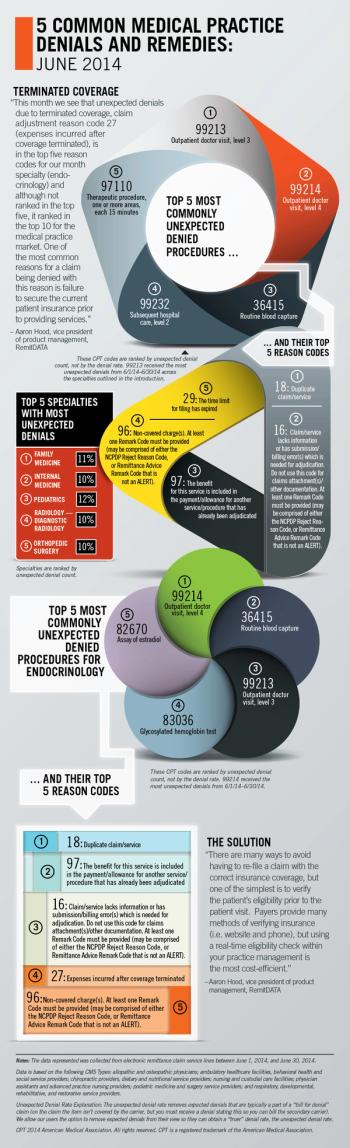
RemitDATA's vice president of product management, Aaron Hood, explores the most common unexpected denials at practices nationwide, focusing on endocrinology.

Small unpaid claims can add up to big problems for your medical practice. Here's how to find the best partner to collect what's owed for your medical services.

As physicians, we have fundamentally failed to clearly communicate to patients what we do, what we cannot do, how we do it, and why it costs what it does.

Though you may have taken a break from ICD-10 planning and prep when news of the delay first broke, it's time to get back to work.

Reviewing the definitions of modifiers first will ensure that applying a modifier goes from a game of chance to a sure thing.

Here are some strategies my medical practice has developed to get those unpaid patient balances off our books.

Performing an audit on your denials will provide a clear picture of where you need to focus your attention in the billing process.

If a CMS proposal goes into effect, primary-care providers are likely to be called on more often to provide follow-up care (primarily, evaluation and management services).

Having a very well written financial policy isn't enough. It's all about staff training and verbal explanations to patients.

One way to ensure patients understand your payment requirements is to ask them to sign a payment policy. Here's a sample policy to consider adapting for your practice.

Americans have changed how they manage their household finances, and medical practices must adjust accordingly.

If your practice accepts medical liens as part of your payer mix, it's a good idea to have a specific follow-up plan in place.
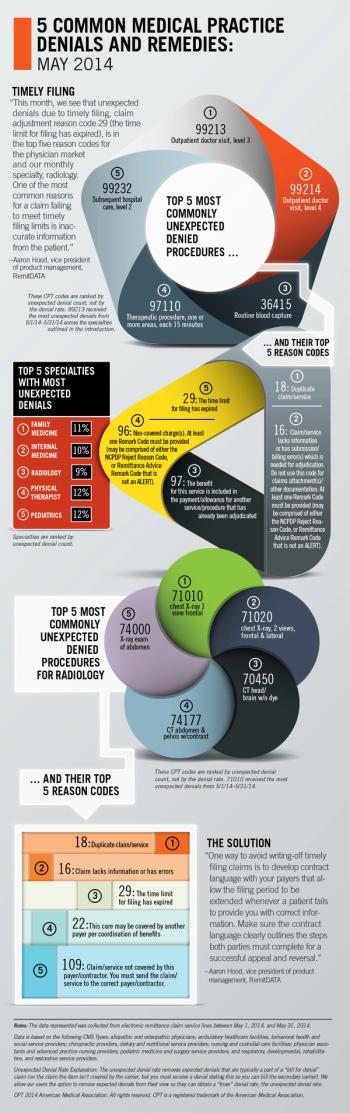
RemitDATA's vice president of product management, Aaron Hood, explores the most common unexpected denials at practices nationwide, with a focus on radiology.

Proposed changes to the Physician Fee Schedule for 2015 will affect calculation of payment rates and potentially misvalued codes.

Except where CPT guidelines state otherwise, follow these four tips to ensure you’re reporting time-based services correctly.

Knowing how to calculate RVU values is critical if you are going to apply them to any other applications. Here's a primer for your medical practice.

If you've ever heard a staff member try to calm an angry patient down on a phone call, you have a great opportunity for training.

Here are 10 tips for Medicare Advantage plans and their aligned physicians to maximize revenue when it comes to Hierarchical Condition Category coding.

When patients refuse to pay their cost-share for healthcare, you have a surprise go-to resource to help get you paid.

When it comes to billing Medicare, you may very well be able to bill one physician incident-to another. Here's how.