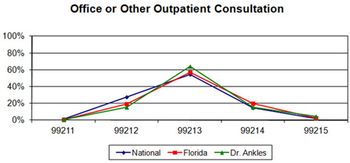
CMS is stepping up efforts to ferret out fraud through its new Center for Program Integrity. Here's what your practice can do to stay below its radar.
CMS is stepping up efforts to ferret out fraud through its new Center for Program Integrity. Here's what your practice can do to stay below its radar.

A natural solution to an increased workload is to recruit for a new physician. Having a plan makes the process much more effective for both the new recruit and your practice.

Every single day, an estimated 10,000 people in this country are turning 65. If you haven't made your practice senior-friendly, now is the time.

All of the parties involved in a physician recruitment agreement need to make sure the documents protect everyone involved to ensure the best outcome.

Receiving maximum practice compensation requires everyone to be on board. If you have a partner who simply won't comply with practice goals that can really hamper your practice. Here's what you can do to motivate your docs.

Here are five key things to keep in mind regarding recruitment agreements between physicians and hospitals.

The break room is the one place people can go for a reprieve from the demands of a busy medical practice. All too often, though, it's a mess. Here are a few tips to help stem the chaos.

Fix the rift between front- and back-office staff with these strategies.
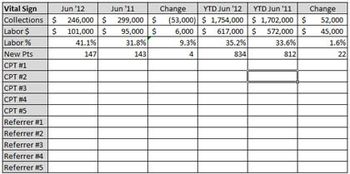
Most physicians have a limited amount of time to monitor the fiscal health of their practices. However, it is possible. Here are five quick measures to make the task easier.

Don't miss out on easy income. Incorporating Medicare's AWV into your care plan helps both your practice and your patients.

Hiring an administrator or practice manager may be one of the most significant hires you make. But how do you hire one successfully?

Whether you've decided to retire, relocate, or retreat from practice, you can reduce the pain for your patients and staff by following these five guidelines.

Whether you practice alone, or in a group, if you're trying to see patients in this pay-for-volume environment and also run the business of your practice, you may be missing out on important opportunities.

Electronic communication between healthcare providers has the potential to radically change healthcare. Referring physicians, consultants, and patients all stand to gain from its use; so why are physicians hesitating?

Reducing patient cycle time and improving patient satisfaction can both be accomplished if you improve your practice's communication channels.

There is much more to billing than just billing; make sure your practice is getting it right.

Many practices fail to appreciate the enormous value of strategic scheduling: a full schedule means a full day of revenue. Because even one missed patient makes a difference, we show you how to stack the deck in your favor.

Many practices make common collection mistakes that when left unattended can sap revenue. Here's what you can do to improve your collection process.

I’m still a doctor, which has never been and will never be a straight 9-to-5 job. Demands, like patients, are unpredictable and often non-negotiable.

Payers are mobilizing their reimbursement models to ensure that they are paying only for "quality" and "efficiency" in medicine.

In the medical world, the way you introduce yourself and others can make or break your relationships - with patients, their families, and your colleagues.

Work flow, technology, and shaking up traditional job duties can all affect staffing needs

Done well, clinical summaries can help you communicate better, satisfy patients, and qualify for the MU bonus.

It’s important to consult with a healthcare lawyer to make sure the methodology being applied to designated health services (DHS) income in your practice is compliant.

It is vital that practices have systematic ways to address patient collections; the following strategies can help your practice collect all that it is due.

Understanding third-party payers can go a long way to making your life easier.

Before selling any product, physicians must consider all legal and ethical limitations.

Tips for testing job skills - before you hire.

The difficulty in collecting payment from patients has only been augmented by the increase in health care plans with high deductibles.

If like many communities, yours has significant numbers of non-English speaking people with whom neither you nor your staff are able to converse, your practice is at a serious disadvantage.