
Having a great collections management policy in place at your practice can serve you very well, and keep your accounts receivable on track.

Having a great collections management policy in place at your practice can serve you very well, and keep your accounts receivable on track.

Close communication with patients is vital to good collections. Send a collection letter after three failed statements, so patients know you mean business.

RemitDATA's Aaron Hood explores the most common unexpected denials at practices nationwide, with a special focus on radiology.

Communication is key as patients are more likely to take their financial obligations seriously when they have a strong relationship with the practice.

Using available data to identify potential high-risk patients before they become high-cost patients can reap rewards for accountable care organizations.

Have an upcoming contract negotiation with a payer? Let Marcia Brauchler give you three key strategies before you sit down at the table.
ICD-10 will be here before you know it. Here's what you need to do before October 1.

Make sure your practice is ready for changes in documentation analysis and quality reporting tied to the ICD-10 coding transition.
The changes in the new ICD-10 coding system will help you do your job better. Here are some changes you'll be happy to meet.

Answers from our coding expert on questions regarding Level 4 documentation and RN reimbursement.

It's possible to be reimbursed for a preventive visit and a problem-focused visit performed on the same day, but proper documentation and coding is critical.

Think coding is hard now? ICD-10 will require far greater specificity and documentation. Here are two ways to start preparing.

You can boost your payment stream significantly by using rejected claims as a learning opportunity. Here's how.

If you're looking to combat rising business costs at your medical practice your best bet is effective coding. Here's how to get started.

Collecting from patients is vital to a practice's bottom line. But often, it is an inconsistent process, done poorly. Here's what you can do about it.
Here are eight simple tips from practice management experts to collect more of the money your practice is owed by patients and payers.
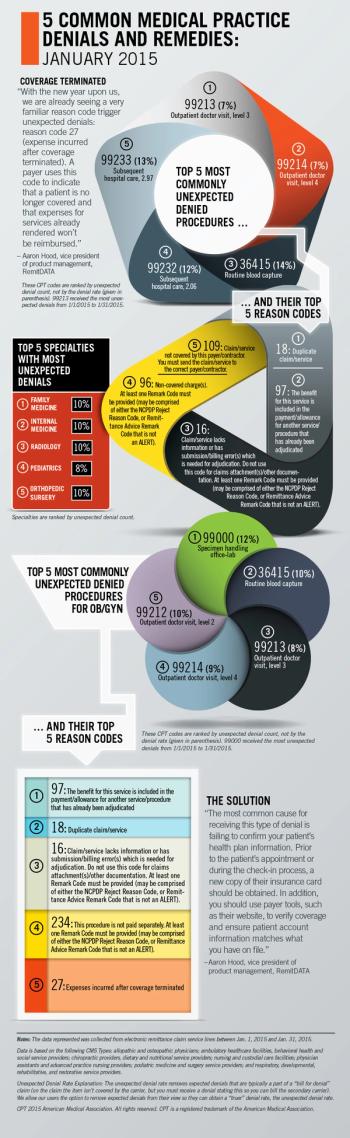
RemitDATA's Aaron Hood explores the most common unexpected denials at practices nationwide, with a special focus on OB/GYN.

Medicare's new value-based modifiers are complex. Here are the important points your practice should know about getting paid for value.

Medicare's value-based modifier is a new fee schedule adjustment that will reward or penalize physicians for quality of care in 2015.

Physicians may find that revised coding guidelines allow their coding and billing to better reflect the documented level of service provided.

Answers from our coding expert on questions regarding discharge code requirements; complex care coordination; and counseling code confusion.

CMS guidance on the 60-day rule can be confusing. Here are some answers to common questions physicians and managers have regarding compliance.
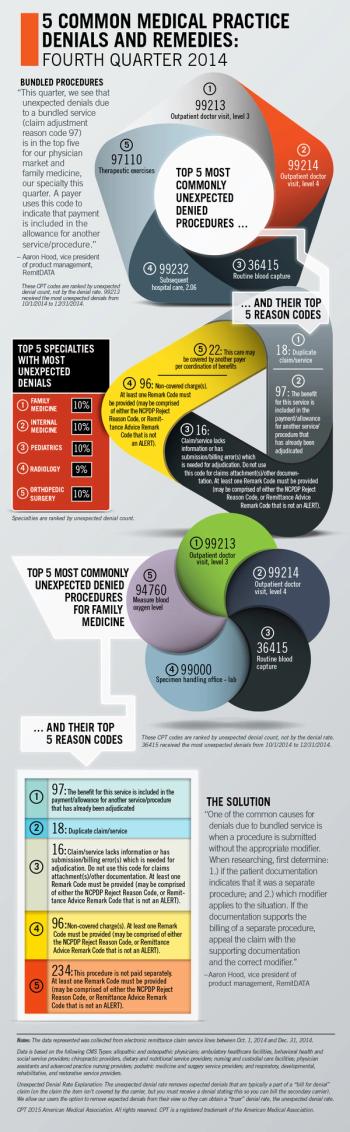
RemitDATA's Aaron Hood explores the most common unexpected denials at practices nationwide, with a special focus on family medicine.

Seen as a prime solution to reducing healthcare costs, bundled payments are on the rise. Here's how to know if they are right for your physicians and practice.

Bundled payments present "significant opportunities" to surgical practices, according to consultant Jamaal Campbell. Here's why.