Payers
Latest News
Latest Videos
CME Content
More News

The alternative practice arrangement is maintaining a stable revenue while also readily adaptable to telemedicine services.

Audits cost providers as much as $1 million annually and damage relationships, but there is an upside a new study says.

Not every financial adviser has your best interests at heart.
Medical practices are struggling to collect patient accounts while honoring payer contracts. Here's what not to do.

Negotiating with payers is not easy, but a challenge worth taking on

As payers and providers strive for value-based care, all sides need to contribute their part toward better data sharing, improving patient outcomes and delivering quality care.

MIPS reporting is more complex now, but the more you invest in quality improvement, the stronger your outcomes will be.

Stop relying on Excel spreadsheets and calendar alerts. Improve your credentialing efficiency, accuracy and speed with technology.

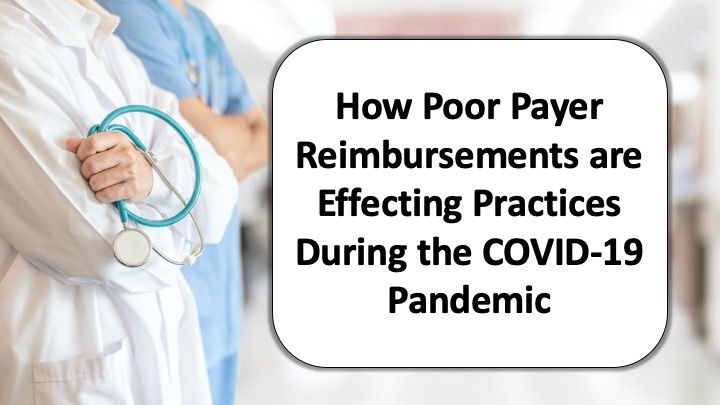
Medical practices continue to be squeezed by increasing costs and decreasing reimbursement, emphasizing the need for better clinical coding and editing technology that can improve claims even before they’re submitted.
It’s crucial to have a robust program for responding to denied claims. Here’s how to build one.

A little attention to small billing mistakes can save your practice big money

Payers don’t dole out equal pay for equal work, so it benefits your physician practice to understand who pays what (so you can negotiate more).

Increase your medical practice's revenue by understanding payer reimbursement tactics.

Community health information exchanges appear to offer many advantages, including increased revenue for physician practices.

Increase patient satisfaction and lift patient collections through transparent patient responsibility

The Affordable Care Act required health insurance plans to include behavioral health coverage, and that has benefits for patients, physicians and payers alike.

A recent court ruling illustrates the risk of failing to place behavioral health coverage needs ahead of financial interest.

Don’t settle for a bad deal. Boost your profits by renegotiating your payer contracts.

Don’t take ‘no’ for an answer: promptly and properly resubmitting claims is crucial to your bottom line.

Ensure your practice’s long-term health by educating patients about their financial responsibility and staff on how to improve medical billing and collections.

Six tips that can help physicians collect on services not covered by third parties.

The ongoing battle to get patients the treatments they need is a major contributor to physician burnout.

In order to justify the Level 4 E/M visit, make sure you have recorded all necessary information-and clearly label it for the payer auditor to easily find.

How to code varies on the circumstances. Many coding scenarios are determined by context-not absolutes.

Credentialing a new provider is a tedious and slow process in which every false step or delay can cost you money. These seven tips can expedite the process.