
Paying primary-care physicians more is a proven winner, but a Michigan study indicates that health plans playing penny-ante get what they pay for.

Paying primary-care physicians more is a proven winner, but a Michigan study indicates that health plans playing penny-ante get what they pay for.

Have an upcoming contract negotiation with a payer? Let Marcia Brauchler give you three key strategies before you sit down at the table.

It's possible to be reimbursed for a preventive visit and a problem-focused visit performed on the same day, but proper documentation and coding is critical.

Can a Supreme Court ruling on teeth whitening make the case against physician exclusion in narrow networks, exchange plans, etc.? Perhaps.

For us, the health insurance companies represent a huge problem. We believe the solution is single payer, and we’re doing something about it.
Here are eight simple tips from practice management experts to collect more of the money your practice is owed by patients and payers.

I hate to think that medicine will become like a cookbook, because there are so many things that just don’t fit inside the box.

CMS' newest shared-savings payment and delivery care model features higher risks and higher rewards. Here's how it differs from current ACO models.
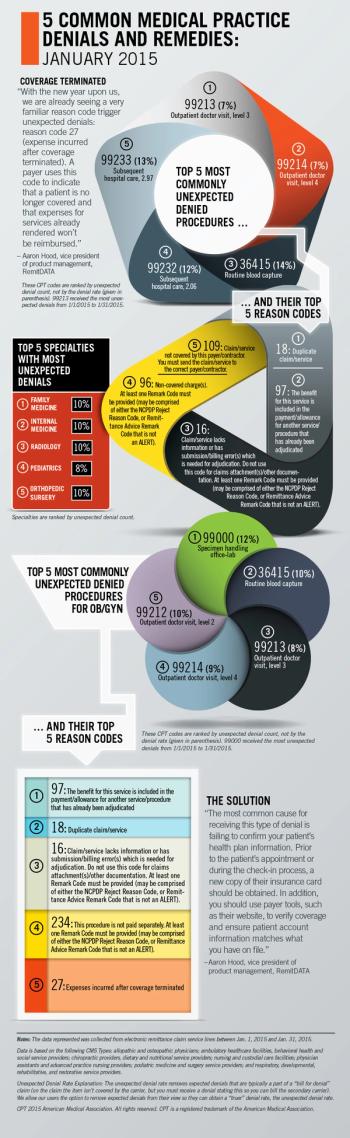
RemitDATA's Aaron Hood explores the most common unexpected denials at practices nationwide, with a special focus on OB/GYN.

Medicare's new value-based modifiers are complex. Here are the important points your practice should know about getting paid for value.

More payers are forming narrow networks and excluding certain physicians from their plans. Here's what your practice should do about it.

Plans offered through the state and federal health insurance exchanges are not the only place narrow networks are cropping up.

Narrow networks have potential negative consequences for physicians who are included or excluded.

An important part of ICD-10 readiness is ensuring all hardware and software is evaluated via a systems inventory.

Physicians may find that revised coding guidelines allow their coding and billing to better reflect the documented level of service provided.

You've budgeted for training and software upgrades, but there are less tangible costs attributed to the ICD-10 transition. Here's how to prepare.

The growing list of payer demands continues to drive medical decision making. It can also impede patient care and hasten physician burnout.
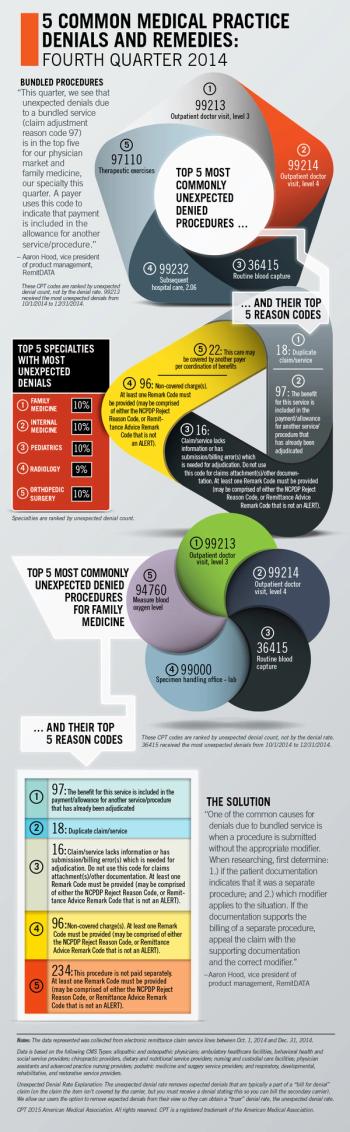
RemitDATA's Aaron Hood explores the most common unexpected denials at practices nationwide, with a special focus on family medicine.

Using RVUs to conduct a cost analysis at your medical practice is not only cheap and easy, it is very effective at assessing the value of your payer contracts.
Five ways your medical practice can better control its payer contracts and boost reimbursement.

Many of the health insurance exchange plans include high deductibles, so getting these patients to pay their portion of your fee is critical.

If your medical practice is not already recognized as a Patient-Centered Medical Home, it may be time to jump on the bandwagon.

The results of our 2014 Fee Schedule Survey are in. Here's a look at some of the key findings, and how physician practices can react.

Test your patient collections knowledge with our interactive quiz, featuring claims and denial data from RemitDATA from the fourth quarter of 2014.

There are several things to consider before making a change from a traditional practice model.