
Independent integrated networks are being driven by independent physician organizations, coalitions, and alliances between physicians themselves.

Independent integrated networks are being driven by independent physician organizations, coalitions, and alliances between physicians themselves.

Monitoring patients remotely is one way to reduce healthcare costs, but it may also facilitate outcome-based reimbursement programs.

Incomplete or inaccurate patient information can set the stage for a claim denial before a visit. Avoid these mistakes at the front desk.

Lack of feedback from back to front office on coding issues perpetuates a cycle of denials. Here are five tips to help get claims paid the first time.

A change in coding for behavioral screenings illustrates how payer payment policies negate any big-data promises of ICD-10.

Sometimes, you have to add a little muscle to the way your staff approaches patient payments and other collections for your medical practice.

Under the HIPAA Omnibus Rule, patients can request a restriction on disclosure of PHI to a payer if they pay out of pocket, in full for a service.

Pay-for-performance programs often set up complex metrics to define quality, when simple solutions to the initial problem would be far more effective.
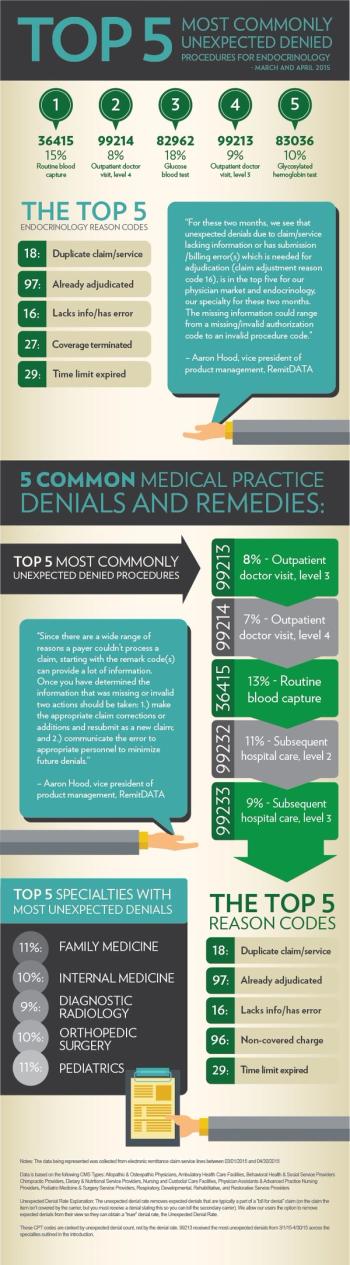
Get insight on the most common unexpected denials at practices nationwide, with a special focus on endocrinology, from RemitDATA.

When it comes to complex payer rules, the most effective course of action is to consult experts for a thorough review of the rules and consequences.
Practices can often feel helpless when it comes to working with payers. Here's how they can change that dynamic and become empowered.

Many practices are running on razor-sharp margins. That puts them at a distinct disadvantage when it comes to dealing with payer-generated work.

Physicians feel at a distinct disadvantage when it comes to working with payers.

Each year, athenahealth ranks payers on how easy they are to work with providers. Here are the top 20 in the "major payer" category for 2015.

Each year, athenahealth ranks payers on how easy they are to work with providers. Here are the top 20 in the "all payers" category for 2015.

Each year, athenahealth ranks payers on how easy they are to work with providers. Here are the top 20 in the Blues category for 2015.

Each year, athenahealth ranks payers on how easy they are to work with providers. Here are the top 20 in the Medicare category for 2015.

Each year, athenahealth ranks payers on how easy they are to work with providers. Here are the top 20 in the Medicaid category for 2015.

Patient satisfaction is doubly important now that it is a payment metric. Make sure you are doing everything possible to get the top scores you deserve.

A little preparation by your practice before reaching the negotiating table with payers could mean a big difference in reimbursements.

One of our payer quality metrics is more like student standardized testing - the intent is good, but the result is a poor indicator of true success.

Stay on top of your claims and denials with these four tips to spot problems early and maximize payer reimbursement.

You may want to help patients experiencing financial difficulties and you can, but be sure to do it the right way to avoid a payer audit and penalty.

From actually locating your payer contracts to making negotiations effective, here are five strategies for your medical practice.

A few trends affecting payer contracts can't really be resolved with better organization, but should be kept in mind.