
Why smart policies must reward smart care by physicians.

Why smart policies must reward smart care by physicians.

Consolidation will probably continue to be a strong trend, but it is not the only available option.

Opportunities to practice telemedicine are emerging due to improved technology and reimbursement. Still, there are some legal issues to consider.

It’s becoming increasingly difficult for private medical practices to thrive. Here’s what’s driving the trend toward consolidation.

ICD-10 diagnosis codes are effective Oct. 1, 2014. Set an implementation budget and timeline. Identify ICD-9/ICD-10 differences. Say goodbye to nonspecific codes.

Interactions between payers and providers tend to focus on rate negotiations and fees for service, but health reform is changing that.

See what CMS owes your medical practice for your services by downloading the the 2013 Medicare Physician Fee Schedule.

New payment models can boost medical practice revenue. Here's how to take advantage.
See where your medical practice stacks up when it comes to reimbursement for top CPT codes on a regional and national scale in our 2012 Fee Schedule Survey results.

Doctors can breathe a sigh of relief as a Medicare pay cut of nearly 30 percent is narrowly averted - at least temporarily.

A recap of this year’s most popular blogs and some of the key lessons that can be learned from each.

Medicare reimbursement could become more problematic the pay cut due to the flawed Sustainable Growth Rate (SGR) formula is not averted.

Physicians continue to drop Medicare patients and it will continue unless something is done to reinvigorate enthusiasm on the part of providers.

The AMA is recommending a “multipronged approach” to slow Medicare cost growth.

Two proposals released last week could lead to higher physician reimbursement.

There are a number of reasons the value-based payment modifier initiative could be an unfair way to determine physician reimbursement. Here are three of them.

Compare your E&M coding patterns with national norms from Medicare. It's a fast way to see if you are out of whack. Translate Medicare's data for your specialty into percentiles for easier comparison.

Perhaps Congress hopes some sort of solution to the SGR will unexpectedly land on its doorstep. And perhaps it finally has - in the form of unspent war funds.

As practices continue to deal with declining reimbursement, federal and commercial payers are exploring new payment models. Here's how to prepare and respond.

The proposal would help physicians dodge a 29.5 percent pay to Medicare services, but it would slam them with other - perhaps more serious - problems.

The Affordable Care Act, signed into law in 2010, is the roadmap for healthcare reform for the next decade. The legislation includes several initiatives that will impact the way physicians operate and change their everyday business practices. Here is a year-by-year outline of the biggest benchmarks that will affect physician practices.

The latest study results from the AMA when it comes to payers and their power in local markets may not be good news to all.

The toughest payers to collect from are your own patients. Don't despair, there are things you can do to get paid.
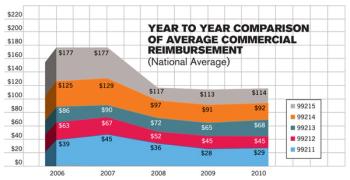
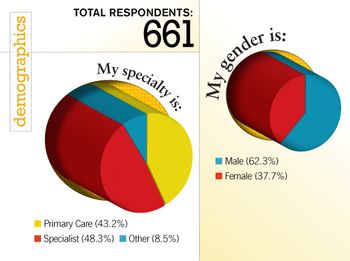
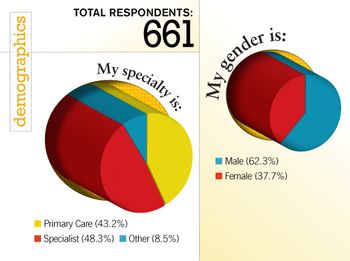
Our 2010 Fee Schedule Survey indicates that with commercial payments narrowly keeping pace with Medicare, practices need to get paid more for the work already being done.